Audrey Stanley's Medical Expenses
Donation protected
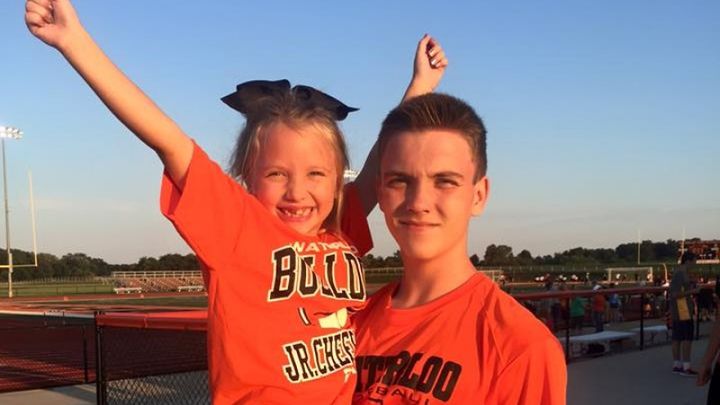
On December 18, 2015, 6 year old Audrey Stanley was diagnosed with a brain tumor and was scheduled for surgery on December 30, 2015. The Surgeons were able to remove the majority of it but could not get a small part in the brain stem (too risky). She was sent to PICU for overnight recovery.
12/31/15 - MRI to follow up on surgery was conducted and looked good. She was sent to the regular Neurology floor for regular recovery. During the overnight hours, she developed breathing complications and could not keep her oxygen up to a stable saturation level.
1/1/16 - Audrey was transported back to the PICU where a team of medical staff went to work to intubate her and get her oxygen back up to a safe level. Once she was stable, she was taken for a head CT where they discovered her first complication, which is a condition known as hydrocephalus (buildup of fluid in the ventricles of the brain). At that point, it was determined that she needed a procedure completed to relieve the pressure called an external ventricular drain (EVD). This is a tube inserted into the top part of her brain to continuously drain the fluid from her brain. This will be in place for at least several days until it is determined whether she needs a permanent drainage put in place (internally). After this procedure was completed, she was monitored for several hours and was still not recovering like they wanted her to. She was sent for another CT scan where it revealed that she had developed another very rare complication of a hemorrhage after surgery was completed. At that point, they determined a second surgery was needed to stop the bleeding. She remained on the ventilator throughout the night. Jason and Melissa were told it might be10 days before we see any real activity out of her.
1/2/16 - Audrey made significant progress and was extubated and breathing on her own again. She was reactive and communicating through eyebrow movement and hand squeezing.
1/3/16 - She continued to make progress. She continued with breathing treatments to suction her mucus out and had multiple chest x-rays to watch her left lung. Breathing treatments were continued throughout the night.
1/4/16 - She would not recover after her mid-morning breathing treatment. Another chest x-ray was completed and determined her entire left lung was collapsed. She could not get her oxygen saturation back up above 90%. At that point, they had to intubate her again. During the intubation, her intracranial pressure (ICP) went up (the pressure in her brain). Audrey was started on a feeding tube since she had not really eaten in about five days other than fluids, etc. she was being given through IV. Breathing with assistance on the ventilator was good now and no brain issues. However, it was determined that her blood was a little thin (again rare), which could have contributed to her brain bleeding. Therefore, she was given some plasma for this to help with coagulation (clotting).
1/5/16 - Audrey is still on the ventilator but has made remarkable progress. Her latest chest x-ray showed that her lung was much clearer than the previous day. She will remain on the ventilator for the day. She is responding through head and eyebrow movements when we talk to her as well as hand squeezing but is still sedated. They will do another chest x-ray in the morning and determine if we will try removing the ventilator again.
12/31/15 - MRI to follow up on surgery was conducted and looked good. She was sent to the regular Neurology floor for regular recovery. During the overnight hours, she developed breathing complications and could not keep her oxygen up to a stable saturation level.
1/1/16 - Audrey was transported back to the PICU where a team of medical staff went to work to intubate her and get her oxygen back up to a safe level. Once she was stable, she was taken for a head CT where they discovered her first complication, which is a condition known as hydrocephalus (buildup of fluid in the ventricles of the brain). At that point, it was determined that she needed a procedure completed to relieve the pressure called an external ventricular drain (EVD). This is a tube inserted into the top part of her brain to continuously drain the fluid from her brain. This will be in place for at least several days until it is determined whether she needs a permanent drainage put in place (internally). After this procedure was completed, she was monitored for several hours and was still not recovering like they wanted her to. She was sent for another CT scan where it revealed that she had developed another very rare complication of a hemorrhage after surgery was completed. At that point, they determined a second surgery was needed to stop the bleeding. She remained on the ventilator throughout the night. Jason and Melissa were told it might be10 days before we see any real activity out of her.
1/2/16 - Audrey made significant progress and was extubated and breathing on her own again. She was reactive and communicating through eyebrow movement and hand squeezing.
1/3/16 - She continued to make progress. She continued with breathing treatments to suction her mucus out and had multiple chest x-rays to watch her left lung. Breathing treatments were continued throughout the night.
1/4/16 - She would not recover after her mid-morning breathing treatment. Another chest x-ray was completed and determined her entire left lung was collapsed. She could not get her oxygen saturation back up above 90%. At that point, they had to intubate her again. During the intubation, her intracranial pressure (ICP) went up (the pressure in her brain). Audrey was started on a feeding tube since she had not really eaten in about five days other than fluids, etc. she was being given through IV. Breathing with assistance on the ventilator was good now and no brain issues. However, it was determined that her blood was a little thin (again rare), which could have contributed to her brain bleeding. Therefore, she was given some plasma for this to help with coagulation (clotting).
1/5/16 - Audrey is still on the ventilator but has made remarkable progress. Her latest chest x-ray showed that her lung was much clearer than the previous day. She will remain on the ventilator for the day. She is responding through head and eyebrow movements when we talk to her as well as hand squeezing but is still sedated. They will do another chest x-ray in the morning and determine if we will try removing the ventilator again.
Organizer and beneficiary
Jodi Horrell
Organizer
Waterloo, IL
Jason Stanley
Beneficiary