
Ashton Scorza's Liver & Heart Disease
Ashton Blake Scorza
Oct. 29, 2013 – Oct. 21, 2014
Think of him as living
In the hearts of those he touched
For nothing loved is ever lost
And he was loved so much.
Below are updates from Ashton’s last admission to the hospital…
Ashton Blake Scorza was born 10/29/13 with a rare disease called Biliary Atresia. This is where the bile ducts that drain bile from the liver into the intestines become scarred and unable to drain causing death with no intervention. He was also born with multiple, life-threatening congenital heart defects. These issues were not known to his parents as they were missed during Anda's pregnancy. Shortly after Ashton was born, his breathing was fast and his blood sugar was low. It was then decided to take him to the NICU (neonatal intensive care unit) where the course of this family's lives was forever changed. In Ashton's 6.5 month life he has undergone 4 heart and liver surgeries, and it will not stop there (there is an 85% chance or greater that he will need a liver transplant and he will have another open heart surgery if not a heart transplant as well). On May 22nd, he underwent the first of a two part open heart surgery and his family is with him as he recovers. Expenses for these new parents had surpassed what they planned for expecting a healthy child. With unpaid leaves from work to be with their son, we are putting this website together to ask for your help. This is a very stressful time in their lives, and the financial burden this has caused is yet another stressor. Please donate if you would like to help Ashton with this difficult journey with his parents. 
---------------------------------------------------------------------------------
UPDATE Thursday 5/22/14
Our new home away from home. The "Bay" of the PCTU
Ashton underwent his 2nd heart surgery but 1st open heart surgery 5/22/14. It is called a "hemi-fontan" operation. This was not the surgery we planned for. We were quite saddened at this news. When they looked at his heart during the surgery, they decided that they don't think his right ventricle will ever be big enough at all to handle all of the blood return from the body thus proceeding with this 2 step surgery. This is the 1st of 2 surgeries instead of being his only open heart surgery. This was totally unexpected. It was not even a possibility that was discussed before they entered the heart. So after this "hemi-fontan", another surgery for the "fontan" procedure on his heart will be around 2 years of age or possibly a heart transplant if the hemi-fontan does not work.
The "fontan" heart usually lasts for 15-30 years after which time, a heart transplant often becomes the next step. Because Ashton's heart condition is very rare and this procedure is typically for children with a small LEFT ventricle and associated problems with the aorta and heart valve, not much is known about this procedure for his condition. Before this surgery, they were hoping to just be able to take out some of the muscle in the right ventricle to make it big enough to handle all of the blood return. The worst case scenario at the time was for him to undergo a 1.5 ventricle repair where they re-route 1 of the 2 major veins that carry blood back from the body to the heart. Unfortunately, neither of these approaches were able to be attempted due to a high risk of them failing so instead, this hemi-fontan procedure he underwent makes Ashton like a 1 ventricle system instead of 2 (like a normal heart) or 1.5. :( This is not what we were expecting or wanting to hear. He was supposed to have the holes in his heart (VSD, ASD) closed and live a pretty normal or entirely normal life from a heart perspective (His liver of course is another issue and most likely will need a liver transplant as a baby or child.)
We are hoping for a miracle for that small chance that his right ventricle will grow or for a better surgical option to surface that is designed for his heart issue specifically rather than making him a "fontan "heart.
His liver is doing okay for the time being. He had his liver surgery called a "Kasai" 12/23/13 where they removed the scarred bile ducts preventing bile flow from the liver into his intestines. The attached his intestine to the liver directly. This surgery was a success but unfortunately, with biliary atresia, damage to the liver often continues necessitating a liver transplant in over 85% of cases. They just hope for the kids to be at least 2 years old when they need the transplant. Ironically, the "fontan" surgery for his heart is also done around 2 years of age usually. If he does need a liver transplant, we pray that the timing does not coincide with his heart surgery. Also, the "hemi-fontan"/ "fontan" makes the liver condition worse too. :(
---------------------------------------------------------------------------------
UPDATES Monday 5/23/14
So Ashton had a terrible night and morning after the surgery. He was bleeding severely immediately after surgery and all night. He had gotten to the intensive care unit from the operating room at 1130 pm and unfortunately was bleeding ever since. He was receiving blood transfusions continuously and was becoming unstable. We were frightened as he was circling the drain and his blood pressure was dropping severely.They were no longer able to keep up with the blood he was losing with the transfusions. He was receiving countless amounts of red blood cells, platelets and plasma.The surgeons were called and after bleeding for nearly 8 hours losing almost twice his entire blood volume, they came in and opened his chest back up at the bedside. It turns out that the chest tube was right on his raw ventricle (raw from surgery)sucking blood right out of it. Also, because the blood in the chest tube was clotting, they were milking the tube to prevent blood from accumulating around the heart and this was creating even more suction and more blood loss. There were no bleeding vessels and with repositioning of the chest tube the bleeding stopped but with much unnecessary trauma to Ashton's little heart. The surgeons had never seen anything like his happen before.
---------------------------------------------------------------------------------
UPDATES Monday 5/26/14
Recovery Day #4
He had a failed extubation (where he came off the ventilator which was breathing for him) 2 days ago and was extubated again about 7 hours ago. The first failed extubation was due to swelling in his airway from the breathing tube, collapse of the small airspaces and too much sedation medication. He's hanging in there, working a little harder to breathe than we would like. But hopefully he'll stay extubated this time.
He's had a constant fever of 101-104 degrees since the very end of his surgery Thursday which came down Sunday morning at 4am, only to come back up at 10am. He had cooled down again just recently but it's too early to tell if it will stay. This can be a number of things from blood clots, brain damage, drug related, blood transfusion related, infection...or a delayed surgical fever (which normally ends after 24-48 hours). They just don't know. Additional tests are being run and infectious disease had been brought on the case. Until we can rule out infection, he will be on some big gun antibiotics.
---------------------------------------------------------------------------------
UPDATES Tuesday 5/27/14
After a miserable 17 hours for Ashton, he was yet again re-intubated (placed back on the ventilator) at 6am this morning (THIRD intubation this admission). He coughed early on while extubated this 2nd time, however stopped even though he was having upper airway secretions. He also didn't gag when they attempted to use suction with a rigid tube. These could be a sign of brain damage (though all other signs seem normal) so Ashton just underwent a head CT scan and we are waiting on those results.
---------------------------------------------------------------------------------
UPDATES Monday 5/28/14
Thankfully Ashton had a normal head CT scan so there was no bleed in his brain! They also did an EEG looking for a seizure and preliminarily it looks negative! Thank goodness! They are thinking his loss of cough and gag is due to his sedative/narcotic medications. Being over medicated was part of the reason he needed to be re-intubated yesterday in addition to a bacterial infection in his lungs. He was placed back on antibiotics.
--------------------------------------------------------------------------------
UPDATES Sunday 6/1/14
Well, last night and this morning Ashton took a step backwards. His temperature is more under control but his white blood count spiked telling us he could have an infection. He is on steroids which can cause it to be slightly elevated but his seems too high to be from the steroids. We're running more tests to find out what's causing this so the right antibiotics can be given. He had a lumbar puncture (spinal tap) yesterday to look for meningitis but thankfully this appears to be negative so far. He has a lot of respiratory secretions building up that he can't cough up (because he's on too many meds that make him too tired to cough.) But he wakes up agitated and kicks, squirms around, and arches his back.... but he doesn't fix the problem with the secretions by coughing. So let's just pray he doesn't tire himself out and have to be re-intubated for the fourth time this admission.
Continued
I was just talking to a mom Friday who's baby has hypoplastic left heart syndrome (which is a much worse condition than hypolastic right heart which Ashton has) that we met in November during their first heart surgeries. Her daughter had the hemi fontan (same as Ashton) and reconstruction of her aorta (which Ashton did not have) on Thursday May 29th which is a week after him and she was eating by bottle completely the next day and the next day after that she got transfered out off the icu onto the floor. When I saw her on friday (the day after her open heart surgery) she was only on 2 liters Nasal cannulq too (that's a small amount). That's how it was supposed to go for Ashton tol! Crazy! She will probably go home in the next day or so. Things are always so hard for him. It's always such a roller coaster ride.
---------------------------------------------------------------------------------
UPDATES Tuesday 6/2/14
They've lost IV access so Ashton is going to the cath lab to get a PICC line, which is a more-long term IV. Say a quick prayer for him and let's hope they can do this without having to re-intubate him.
Just before leaving his room for the procedure.
On his way down to cath lab

Ashton's back. PICC line was put in under sedation with no complications and he was NOT re-intubated! When they sedate him for procedures, you always run the risk of re-intubation. His fever has subsided and his heart function looks good. His lungs are better and they have come down a little on the oxygen. Now we're just slowly weaning him off his narcotic and sedative meds. He's been on them for so long that they are giving him methadone to help wean him off the iv drips to help prevent him from going through withdrawal... The methadone will have to come off eventually too. if everything goes well from here on out we should be home in three weeks or so.
---------------------------------------------------------------------------------
Updates Tuesday 6/3/14
When being administered sedatives everytime you appear to be agitated...wouldn't that make a perfect time to start teething? Ashton has a tooth coming in and rubbing his tongue over it seems to help.
---------------------------------------------------------------------------------
Updates Sunday 6/8/14
Ashton's showing signs of his old playful self! He's TRYING to smile and is kicking his legs playfully again (we think he's going to be a soccer player).
It's been a rough 4 days since I last updated everyone. His PICC line was put in Tuesday with no problems. Then Wednesday they switched his diuretics from IV to oral and that did not go well. In just a couple hours he puffed up and was more swollen than he was when he got out of surgery. In 2 days he gained 1kg of weight! His breathing became harder and harder. Fluid began building up around his lungs. The diuretics were switched back to IV and were increased. That was not working, so he was placed on a continuous IV drip. With poor results, he was put on the maximum dosages and a third diuretic was added. Last night was his first day of losing weight (which was all fluid he had been retaining).
Yesterday it was decided to give Ashton another blood transfusion. They ran another type and screen test to make sure of what type of blood he can receive. It turns out while he was bleeding out for 8 hours immediately after his surgery and given transfusion after transfusion to the point of where they couldn't keep up, Ashton formed 2 new antibodies. This limits who he can get blood from (& makes it harder to get). Luckily that shouldn't effect him if he needs a liver transplant.
Today's x-ray showed a lot of fluid in the left side of his chest.The worry here was "Chyle" which can accumulate around the lungs if lymphatic ducts are damaged during heart surgery. Because lymphatic fluid is important for immune function, this creates an immune suppressed state as well as metabolic issues if it is leaking. It presents itself shortly after oral feeds resume (just what happened with Ashton). This is very rare, but rare is Ashton's middle name these days. 50% of the time these damaged ducts will close on their own; for those who don't, a surgery is needed. A chest tube was placed this afternoon to drain this fluid and it appears to be, for the most part, clear liquid (which is good news). To be sure, they will watch the output closely and run tests if necessary to rule out Chyle if they aren't sure.
Becoming more alert and for the first time since his surgery 5/22 recognizes his Mom & Dad... and got excited about it (as excited as he can anyways, still very sleepy). He smiled several times in a short period of time :)
---------------------------------------------------------------------------------
UPDATES Monday 6/9/14
Yesterday we mentioned Ashton being at risk for Chyle (chylothorax). Tests have come back showing this is the case. We are waiting to talk to the doctors to see what are approach will be. So basically Ashton's lymphatic ducts are leaking. The fluids that are coming out into his chest cavity consist of lymphocytes, proteins, coagulation factors, and antibodies... All bad things to be losing. Diet alone can help 50% of patients with chyle, the other half need surgery. With this going on we'll be here a while longer. This will make him much more susceptible to infections, have problems with malnutrition and electrolytes. This is bad news. We'll keep you posted.
Continued
Sorry for the late update. We spoke to the cardiologists and they are watching how much fluid leaks over the next 24-48 hours and that will determine how they will treat Ashton's Chyle. Leaks fewer than 40ml per kg per day they proceed by changing his diet to a low fat diet consisting of medium change triglycerides and hope that over the next 6 weeks the ducts repair themselves. If he leaks more, they will first stop feeding him and put him back on nutrition through his iv and if that doesn't work then an additional surgery would be needed. So far it seems to be leaking under that 40 mark, but time will tell. Goodnight everyone. We'll keep you posted when we know more.
---------------------------------------------------------------------------------
UPDATES Sunday 6/22/14
Ashton is undergoing yet another surgery (they just took him down to the operating room). Please say a quick prayer for him. His sternum has not healed properly and has been causing Ashton a great deal of pain. Unfortunately this is the best solution. They'll be going through the same incision and re-opening his chest. This requires him going on the ventilator for the fourth time this admission. We'll keep you posted with any updates.
Continued
Ashton is back from surgery! They are just trying to get the breathing tube out. Please pray for it to come out and stay out! You guys won't believe this. When they opened him up, his sternum was completely open. The surgeon was amazed at how he was compensating with his breathing with it not even attached. Because it was completely healed on the outside. The bone did not look infected and it looked healthy. He placed sternal wires this time. He said that maybe some strong coughs popped one suture then the rest followed. He is such a strong boy the surgeon said. He said if he was tolerating that he should do just fine now. That seems to have been the reason for his breathing issues.
Continued
Ashton's finally resting comfortably! His numbers are the best they've been all week and he's back on the same meds as before with nothing new. No drips! Just a chest tube!! Too bad it took him 31 days to get here but finally he can start his recovery the right way.
---------------------------------------------------------------------------------
UPDATES Friday 7/11/14
They just took him for the heart cath, say a prayer that they find a solution to his problems and that it isn't anything major.
---------------------------------------------------------------------------------
UPDATES Saturday 7/12/14
Today it became very apparent that Ashton will not be able to get better with medical management and needs a heart transplant. The issue is getting him listed. Tests need to be done to rule out lung disease as he has been on lung support this entire admission and if this is not something a new heart will correct, they won't give him a new heart. And he needs to be more stable to get this test so he needs to bounce back from this episode. Then if and when he's listed he has to survive until there is a donor that matches exactly what he needs. 1 in 4 die waiting... and again that's if he meets criteria to get listed (ie his other organs are fine, lungs and liver). So please pray that he gets stable by the end of the week so he can get his lung tests...and that his lungs will be ok and he will meet criteria and get on the heart transplant list.
---------------------------------------------------------------------------------
UPDATES Wednesday 7/16/14
After a very difficult night, Ashton has been re-intubated. It was hard to see him decline. Hopefully they can get his fluid balance and lung issues under control now that he won't have to work as hard having the ventilator breath for him. As he quickly deteriorated, please pray that he will become more stable and will be able to come off of the vent and that this is not a bad sign of things to come.
Continued
Ashton is having a rough course. Shortly after 1pm (during our meeting with all the doctors) his oxygen saturations dropped into the 50's not coming back up. The rapid response team came and treating him almost as if he was coding (ie his heart stopping which it didn't). After 2 hours his vitals bounced back up, not all the way up to where they were this morning after intubating (low 80's), but low 70's... which they are comfortable with for now.
---------------------------------------------------------------------------------
UPDATES Thursday 7/17/14
He's back from his chest CT scan, doing the same as before (nothing impressive, but stable). No results yet, and very well may not get any until tomorrow. We'll keep you posted.
---------------------------------------------------------------------------------
UPDATES Saturday 7/19/14
Basically they went back to the cath lab to help rule out lung disease to get on transplant list. But they were also hoping to get some answers. With the pressures in his heart being so high they expected there to be venous collaterals, and there were. Basically the heart creates these pop off veins which go from his upper heart down and bypass the lungs and go to the pulmonary veins instead, therefore not picking up oxygen thus lowering his body's oxygen saturations. They found a main branch which had 3 veins stemming from it and plugged those 3 veins which is only a temporary fix. Because of the diastolic pressures, these collaterals will continue to form. He had a large branch that formed this time so was easier to plug, but there are several smaller collaterals and eventually more and more of those will form. The root problem is his diastolic dysfunction, and if that does not heal over time the only solution is a heart transplant. From what they saw, lung disease is not the problem here. The heart transplant team will continue their discussions and hopefully be able to list him within the next week.
He's doing worse today. After his heart catheterization we saw some promising signs, but those were short lived. And today he's having a hard time keeping his blood pressure up.
Continued
Ashton had a lot of Venus collaterals; this is his imagining before plugging them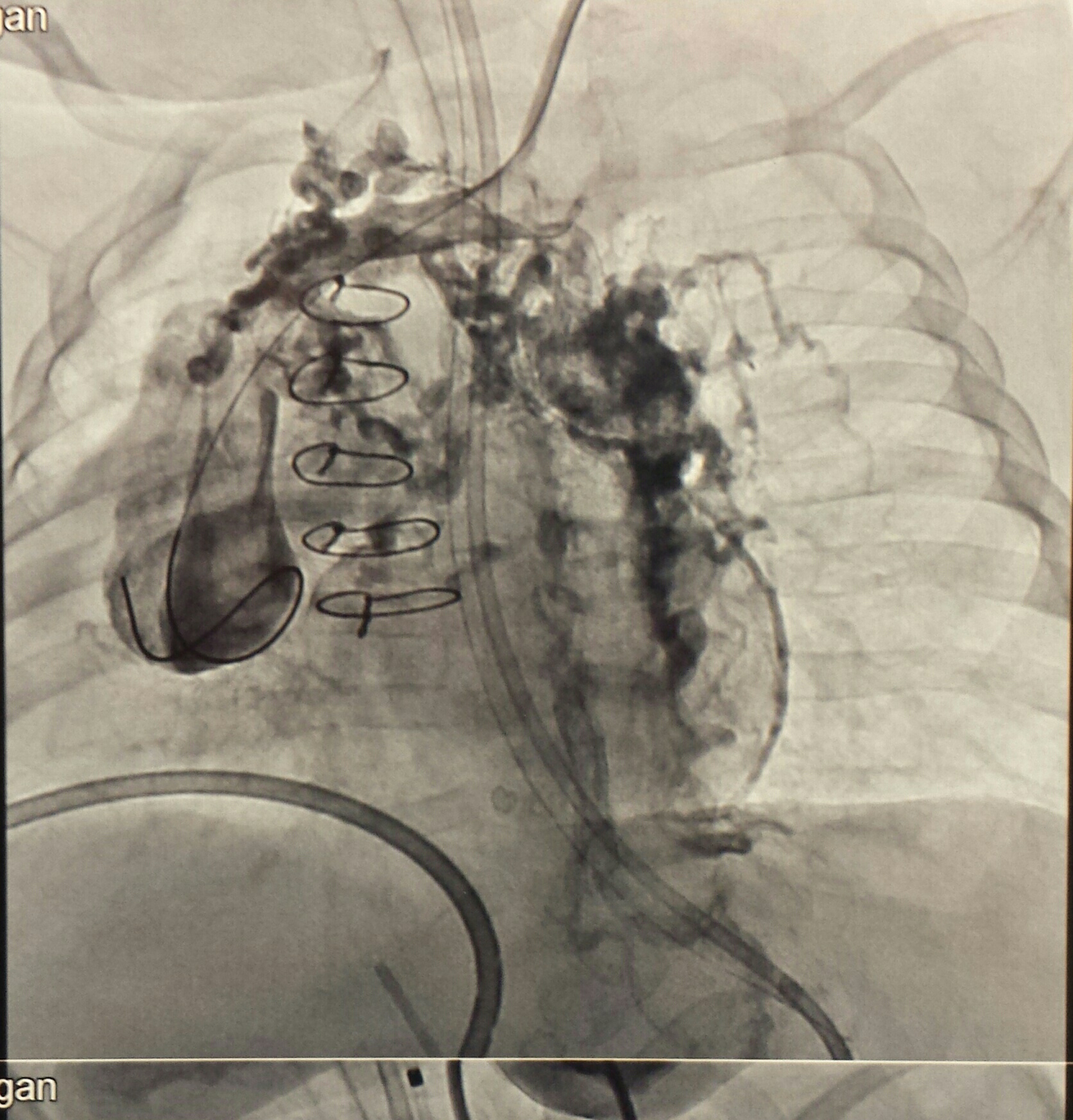
Here's after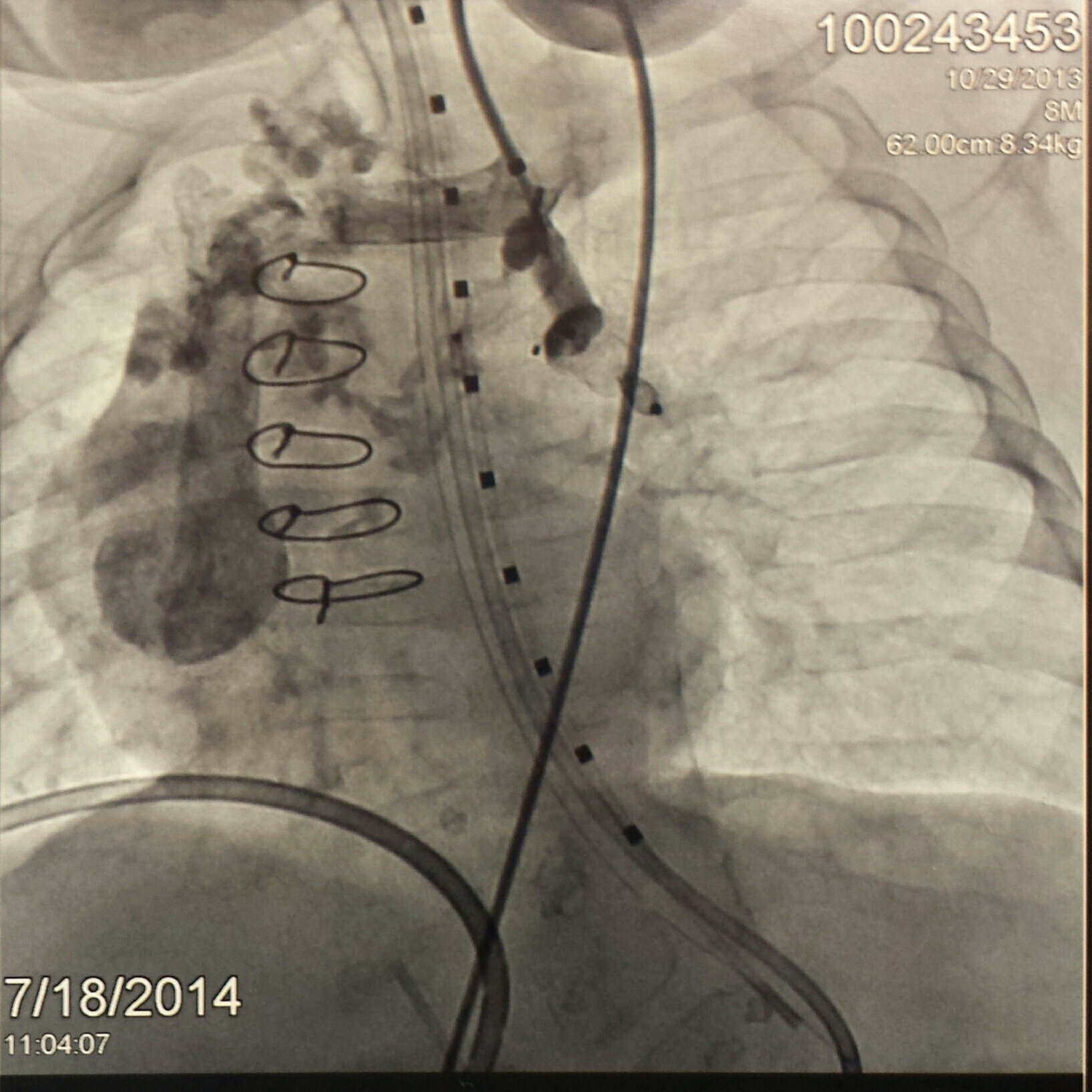
---------------------------------------------------------------------------------
UPDATES Sunday 7/20/14
He's stable, but nothing impressive. Just trying to wean down some of the meds that were recently added as well as his respiratory support. He's been intravascularly dry (blood volume) since he's on all his diuretics. And they want to try not to give him more blood transfusions since he can form antibodies and that could weaken the selection of donors for a heart transplant. So he's been getting albumin instead of blood. This is a blood protein that binds with water thus increasing his blood volume allowing the diuretics to continue to help reduce his fluid accumulation in the right places. That seems to be working well so we're happy with that. As for getting on the transplant list, there are a few more things the team needs and they will have an answer for us on Friday. We tried to push that date up but these meetings involve a lot of people; transplant team physicians, social workers, psych evaluators, financial people, etc...but he will be discussed amongst the team throughout the week.
Continued
How do you like our matching hairdos?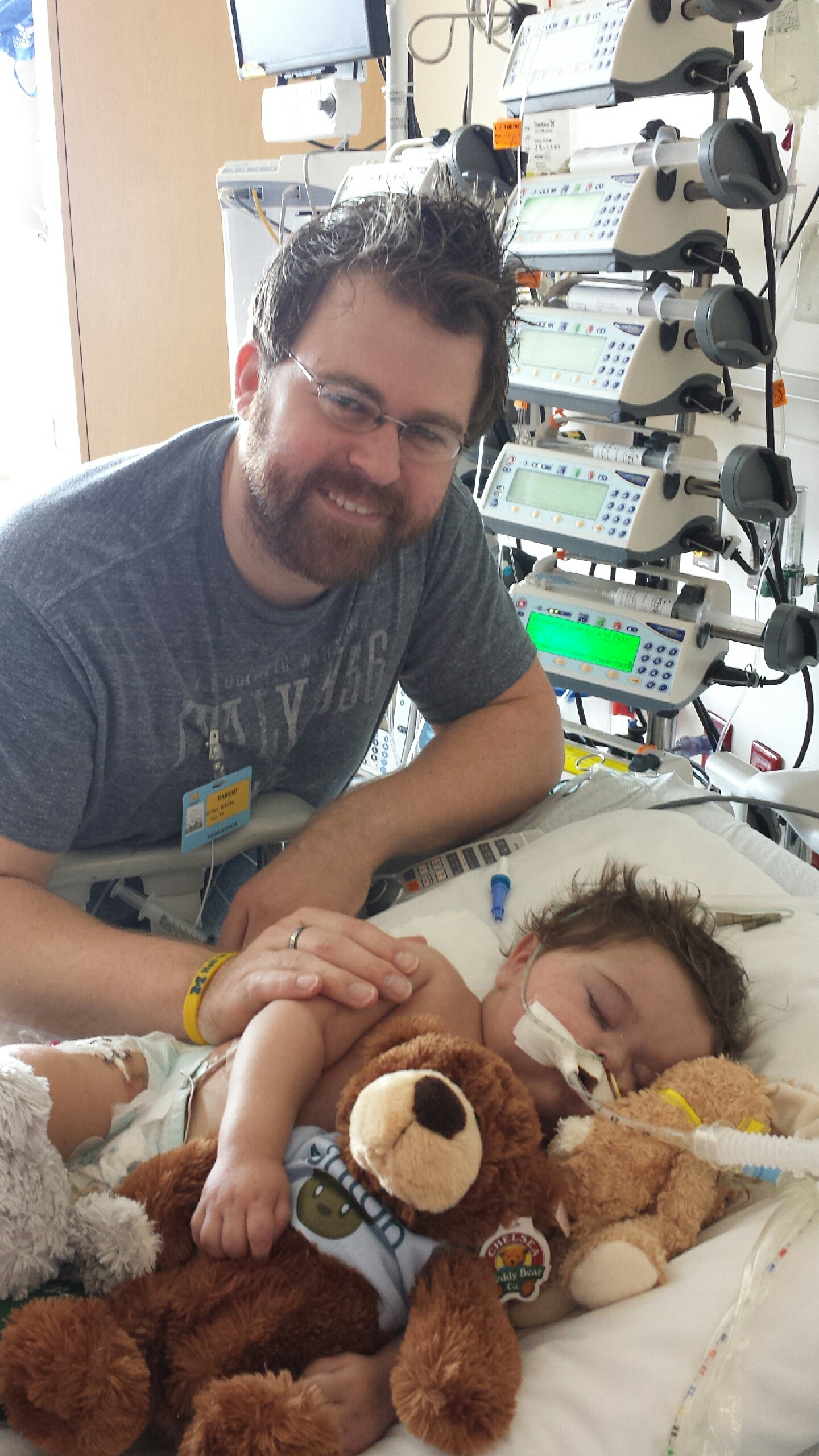
Continued
Hi everyone. Sorry I haven't sent out an update in a very long time, we've been going through a lot here. Today is Ashton's 59th day in the hospital. Ashton has not recovered as we had hoped and is now in diastolic heart failure. With his physiology, his right and left ventricle act as a single ventricle and it is not relaxing as it pumps. There are medications to help a heart pump, but none to help it relax. Because of this diastolic dysfunction his other organs are taking a hit and he is suffering a great deal. So with this news his only option is to have a heart transplant. He is undergoing an extensive workup to make sure his other organs are healthy (which so far they are) to see if he is a candidate for a heart transplant. The transplant team will meet this Friday and discuss whether they think he can survive a transplant and that will determine whether they list him or not. 1 in 4 children die waiting for a heart. And if he gets a transplant that unfortunately comes with a lot of problems as well as a 10 year survival rate. Of course a lot of research is being done in this area and 10 years may be just the amount time for them to come up with what he and so many other children need.
---------------------------------------------------------------------------------
UPDATES Wednesday 7/23/14
Hi guys. He's doing a little better, still in heart failure obviously. We had a family meeting yesterday where they went over the process. Today we met with social work, the transplant surgeon, and are waiting on the phycologist. Ashton had more labs drawn and sent out. The transplant team meets Friday and will make their decision to list him or not. Then provided all the labs are back and insurance company clears him for transplant saying they'll pay...Ashton will be listed. If there is a delay with some of that he'll be listed early next week. For some unknown reason no one is in a hurry to get these things done out here at U of M.
---------------------------------------------------------------------------------
UPDATES Saturday 8/9/14
Here's a picture of Ashton today
Here's an update on Ashton: He is up 1.43kg from his dry weight. He's getting so much fluid from food and meds that he's not peeing enough to stay balanced. We changed some of the concentrations of his iv meds to reduce his overall fluid intake as well as increased his food calories so we could go down on the volume. That's all happening today so it will be a couple of days to see if it helps. His hemoglobin has been at 8 for a few days which is very low. They still check his blood 4 times a day so that number will only drop. Unfortunately today they decided to give him blood in order to increase this number and also in hopes of perfusing his kidneys to help him get rid of more fluid. Blood transfusions put people at risk of forming antibodies which further limit what heart he can accept for transplant, so let's pray he doesn't develop any antibodies from this transfusion. So far this admission he had formed 2 that we know of. Those 2 shouldn't limit which heart he can get.
---------------------------------------------------------------------------------
UPDATES Saturday 8/16/14
Ashton was positive 90 today and up 45 grams (now 1.22kg over his dry weight) so he's quite overloaded. He blew through one of his peripherals so has just one left. They scheduled him to go to the cath lab to replace his picc line first case tomorrow (7:30am) so let's pray he keeps his access until then.
---------------------------------------------------------------------------------
UPDATES Tuesday 8/26/14
Update on Ashton:
In the upcoming days we will be transferring Ashton's care to Boston Children's Hospital. We will keep you posted as we know more.
Six weeks ago we requested second opinions from 3 other institutions (all before talk of transplant started here). Two hospitals came back saying they would do a biventricular repair closing the ASD & VSD. The third institution said they would list him for transplant. As we were waiting on the second opinions to come back, U of M decided to list Ashton for a heart transplant. So between four institutions two felt transplant would be best, and two felt surgical repair would be best, a 50/50 split.
Ashton has been on the heart transplant list for a month and his health is severely declining. He is maxed out on diuretics and his kidney function is nearing failure. Within a week, from a renal standpoint, he will be too sick to be on the transplant list. At that point he can undergo dialysis after which he must be able to prove he is not dialysis dependant in order to get back on the transplant list. And the odds of that happening are very unlikely.
As the weeks have gone by, the team of doctors here have been in close contact with one of the institutions electing to do surgery, Boston Children's Hospital. Boston is the top ranked program for peds cardiology and biventricular repairs are their niche. Boston had suggested an MRI and repeat echo. Much to the U of M team's surprise, the findings do in fact explain why Ashton is so much sicker than he should be with simply diastolic dysfunction. U of M is the 6th ranked program for peds cardiology and they now feel we would be in better hands at Boston. And given his current clinical status, being a week away from being too sick to list, surgery will give him the best shot at survival. It is a very high risk surgery but U of M feels if anyone can do it, Boston can.
---------------------------------------------------------------------------------
UPDATES Thursday 9/4/14
We're now in Boston and they are taking Ashton to the cath lab...
Unfortunately his surgery got bumped. It was supposed to be today, then it was scheduled for tomorrow, but the head surgeon is heading out of the country tonight. And they want the best for the job (as do we) so Ashton will be having his open heart surgery next week Tuesday.
---------------------------------------------------------------------------------
UPDATES Wednesday 9/10/14
Here's an update on Ashton:
His surgery went well yesterday. He was in the OR from 4:30pm-2am. They did all the repairs without complication (took off pulmonary artery band and patched artery, broke down hemi fontan circuit and reconnected SVC to right atrium, closed VSD and ASD, removed tricuspid valve and made cuts in right ventricle to help it relax and open apex, and finally reattach tricuspid valve). Next day is critical to make sure kidneys and liver don't go into failure as he was on bypass. Then it'll be about a month until we can tell if his diastolic dysfunction improves (which was the reason he was on the heart transplant list to begin with). We are so thrilled they did the surgery University of Michigan was supposed to do three months ago and took down the surgery they did do. We're definitely in the right place. His head is smaller with less swelling, he hardly looks puffy (he was getting more puffy each day in the last two months before this surgery as he was getting more and more fluid overloaded). The pressures in his heart immediately following his open operation were normal (around 8, and prior to yesterday they were 20). They have gone up to 10-13 today but still a ton better than they were and everyone is happy with that. We're not out of the woods yet, but so far things are going extremely well and he is impressing everyone! I'll keep you posted with his progress.
I have pictures of Ashton, but it is graphic. If you would like to see how he looks today let me know and I'll send it, just wanted to fare warn everyone before sending it. (His chest was left open after surgery though there is a bandage over it, and he is fully sedated and has a lot of tubes and wires coming out of him, but he looks better already).
---------------------------------------------------------------------------------
UPDATES Monday 9/15/14
Hi guys. So after a rocky weekend Ashton is doing better. We had a scare with his urine output and he was 400 positive Friday then another 300 positive Saturday. With him being so fluid up his heart pressures have been high and they are continuing to leave his chest open (they were going to close it this past Saturday). The team was worried about possible infection or even being septic. His platelets were on the low side of 120 when we transferred here and over the weekend the dropped to 50, then to 17! Then the scare of DIC (severe clotting issues) came which could be fatal. They took him off his heparin drip (blood thinner) in hopes of that being the reason for his dropping platelet levels and thankfully the platelets came up a little bit to 24. Contributing to this may be some level of liver dysfunction after the surgery and a small clot in his vein he has consuming some of his platelets as well (we found out he has this small blood clot in his IVC which they think is from his picc line that he had for nearly 2 months). They started him on a different blood thinner and hopefully the clot will dissolve itself (again scary that this even happened). It's been such a tough weekend for Ashton, but hopefully the storm has passed. He was negative 260 yesterday and is on track to be negative today. The team is trying to stay one step ahead of him and are constantly changing his medications and the dosages he's on. They are so much better here than at University of Michigan, we're definitely in the right place for him (this is Harvard's teaching hospital and they are ranked #1 after all). Still a very long road ahead. They hope to close his chest towards the end of the week and their immediate goal is get him negative. We'll keep you posted with his progress when we can, he's keeping everyone on their toes here and things are constantly changing.
---------------------------------------------------------------------------------
UPDATES Tuesday 9/16/14
Last picture with an open chest, they're closing it now
---------------------------------------------------------------------------------
UPDATES Thursday 9/25/14
Here's a picture of Ashton with Dr. DiNardo. This was the attending this week during a crucial time for Ashton. He made changes in his care that helped Ashton tremendously. His first day on he gave a breakdown of his plan for the week and we were very impressed by how well thought out it was. He made some pretty big changes from his first day on and Ashton's amazing progress this week was in part because of Dr. DiNardo. Very nice man!
---------------------------------------------------------------------------------
UPDATES Wednesday 10/8/14
Here's Ashton today. We have been having our ups and downs with him and scares. They took out his chest tubes (one yesterday and one the day before) but the fluid is re-accumulating. They figured it would but they were hoping the body would reabsorb the fluid (small chance). They have to put in smaller ones now.
He had really low bps again a few nights ago out of nowhere and had to escalate his blood pressure support dramatically which we have come down a little since thank goodness. He just doesn't pee hardly with normal blood pressures. His kidneys weren't this sensitive preop. And he has these areas on his legs that are red and they aren't sure what it is. At first it looked like it could be cellulitis but it is changing in appearance and it could be a vasculitis. Derm is not sure either so they may end up doing a biopsy. He has poor wound healing and his chest tube sites are all macerated and have gaping holes. He needs better nutrition but he has been on so much meds that they were restricting that to help with his fluid balance. Every day is a new adventure, and he is so tricky.
The good news is that we have been weaning the ventilator so that is great! They will trial him with extubation late this weekend or early next week! I hope he can handle it so that he can avoid getting a tracheostomy. We sure pray that it works and that he will only need the cpap mask for a short period of time. He has been weaning off his sedation nicely too and is awake and his eyes have meaning once again!
---------------------------------------------------------------------------------
UPDATES Thursday 10/9/14
Ashton could use some prayers right now. He's become septic. He was not his usual self today and out of nowhere his tidal volumes (amount of air he breathes in each breath) dropped in half. His blood pressure dropped too as did his heart rate and his rectal temp dropped to 33.1 Celsius (91.6 F). Many kids this sick to begin with don't survive sepsis so please pray he can bounce back from this. They're throwing a lot of Antibiotics and an anti-fungal medication at him. Both hit his already damaged kidneys and liver, but the team needs to cover everything. His intestines aren't moving well (ileus vs low grade small bowel obstruction) so this is either the inciting event for the sepsis or the result of sepsis from something else like a line infection or something. He is not breathing on his own anymore like he was and he is on a lot of respiratory support. We were supposed to extubate (take out breathing tube) him this weekend or early next week, but that will no longer be the case. He's such a fighter, but he's been fighting for so long. Please pray he has it in him to get through this. This is the last thing he needed right now with how tenuous and sick he is.
---------------------------------------------------------------------------------
UPDATES Friday 10/10/14
In the last 12 hours Ashton has been getting much worse. They are running test after test trying to figure out what's happening. The worry is he may be in acute fulminant liver failure. The liver issues may be secondary to whatever infection he has or due to the clot he has that is getting bigger or some obstructive process in his bowels potentially, but if that is in fact the case, it could be fatal in a matter of days. His total bilirubin levels jumped from 1.0 to 8, then 15 in these 12 hours. His lfts from normal ( 50s) to 7500 and 1500. Surgery is going to talk to the liver transplant team today for their thoughts. Usually in these circumstances, there is no time to wait for a liver but if I am, or other family, is a match that may be a possibility if time allows. Though it looks like liver failure, let's pray it's not.
---------------------------------------------------------------------------------
UPDATES Saturday 10/11/14
Ashton is getting worse. Ashton is fluid up a ton now. We're waiting to talk to the team about another ventilation device that can help with this since he is near maxed out on respiratory support with the current equipment. Or they may want to go to ecmo (like dialysis machine) that oxygenates the blood for him instead of needing so much vent support to oxygenate his blood. But that could send him into kidney or liver failure as neither are doing well currently and the high risk of stroke. His kidneys are not working well and he's hardly urinating. His liver levels hit a plateau yesterday, but got worse today. He has all the signs of liver failure. He's not doing well and is only getting worse quickly.
Continued
Today was not the day of recovery we were going for. A whole new set of battles happened. Ashton had fluid in his lungs so the surgical fellow went to put a chest tube in to drain it. While inserting the tube Ashton began to bleed nonstop and he was losing blood fast. They feared the chest tube went into a blood vessel. They did an emergent echo to look to see where the chest tube went to but couldn't tell. They called his surgeon and he said they couldn't operate because Ashton would bleed out and die on the table. The only hope was to go to the cath lab to see if they could inject contrast and see where the chest tube went to and possibly coil the vessel so he would stop bleeding. During the cath the bleeding stopped and they were able to pull out the chest tube. During this event he lost all of the blood in his body and thankfully they were able to keep up with it and it was all replaced. He's back in the ICU and stable but this was not the setback he needed. This was completely separate from his sepsis and he'll have to recover from this on top of whatever infection he has. The ICU doctor is surprised he lived through the events today but is not as optimistic about him beating the infection he has and recovering from his liver and kidney damage. We will see. We can't believe his heart didn't stop today, thank God. We'll keep you posted.
---------------------------------------------------------------------------------
UPDATES Wednesday 10/15/14
Ashton is not recovering from his septic or hemorrhagic shock. He was doing better than anyone would have hoped for in the days after those events, but now is deteriorating. They said it was a miracle he survived and was doing better over the weekend. During these episodes though he received a ton of fluid and his kidney function has worsened so he is not able to pee that out. With how his right atrial pressures are because of the extra fluid on an already stiff heart, we have to get his blood pressure much higher to get blood flow to his kidneys so he can pee which is just not possible right now with how high a blood pressure he needs. That's the problem with right sided heart issues. They were getting so much better and they were shocked at how well the surgery worked before the infection and septic shock hit and then the complication of hitting an artery during the chest tube placement and hemorrhaging. These two events necessitated a a lot of fluid and blood and getting extremely fluid overloaded as a result which means higher vent settings and then that causes more fluid retention because its raising his right heart pressure. He should weigh 23 lbs but has an additional 10 lbs of fluid. Nothing seems to be helping. The team was hoping to give him until Friday to recover but as of yesterday evening his urine output has stopped. The surgery team will be placing a PD drain in his abdomen in hopes that they can drain some of this fluid which they are not even sure he has any pocket of fluid to drain but they have to try. If that doesn't work he will go on dialysis tomorrow for fluid removal. The team is not very optimistic about this. If this doesn't work, they will have exhausted all their options for Ashton. Last week this time we were planning on extubating him over the weekend and talking about how great his recovery was going, what a turn of events this has been. Please pray that Ashton can get this fluid off...his life depends on it.
---------------------------------------------------------------------------------
UPDATES Tuesday 10/21/14
It is with a heavy heart that I write this text. Ashton passed away today. He fought 9 of his 12 months of life in the hospital. Hurdle after hurdle he bounced back. He was an amazing child. Two weeks ago he was well on his way to recovery and we were planning to extubate (take breathing tube out) him after being on the ventilator for three months. Then he went into septic shock from a severe infection. Two days later a chest tube was placed to drain fluid that was collecting inside his body and an artery was hit. Ashton then went into hemorrhagic shock. No one thought he would survive the night, but he did. They said it was a miracle. With these episodes happening back to back Ashton simply didn't have the reserves to bounce back this time. His kidneys and liver began to fail. He was placed on ECMO since his heart wouldn't tolerate fluid shifts dialysis would create in a last effort to save him. Never during any one of the tons of episodes Ashton underwent did his heart stop. Other infants code under lesser things. But Ashton was like no other kid. He just kept fighting and he just needed us to be the ones to tell him it's ok to go. Today he is no longer in pain, no longer with the many scars his earthly body has, Ashton is now with God. We made him comfortable and stopped the treatment and he became a forever angel at 3:03 pm. Thank you for all of your thoughts and prayers during these last twelve months. God most certainly worked miracles with him in the past, but today decided to bring him home.
---------------------------------------------------------------------------------
Hi everyone. Here is the information for Ashton's services this week. We just solidified these plans so thought to pass them on to you.
Wake/Visitation:
Tuesday 5pm-8pm
Langeland Funeral Home
Westside Chapel
3926 S. 9th Street
Kalamazoo, MI 49009
Funeral Service:
Wednesday at 11am
Kalamazoo First Presbyterian Church
321 W South Street
Kalamazoo, MI 49007
Burial:
Following funeral service
Mt Olivet Cemetery-Mausoleum
2003 Mt Olivet Road
Kalamazoo, MI 49004