Kerie's Breast Cancer Fund
Donation protected
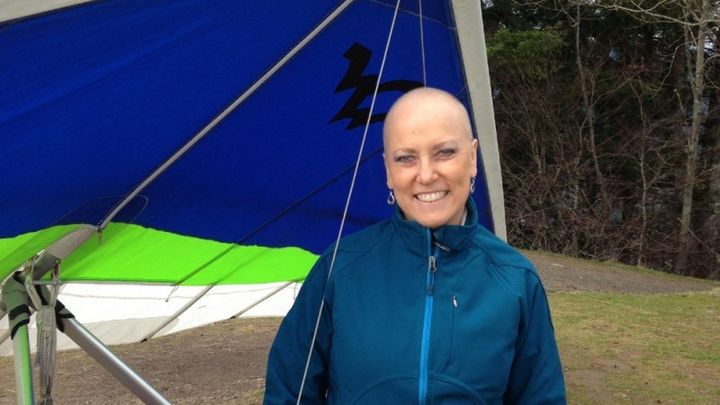
My dear flying friend Kerie Swepston (we hang glide together) has been going through treatment for an aggressive form of breast cancer since October 2013. Although she has good insurance her out of pocket medical expenses are already reaching $10,000. Kerie doesn't know that I'm setting up this gofundme site. Kerie and Aaron have been married 25 years and have two wonderful kids, Jade and Jaguar. Kerie and her husband Aaron are used to being the "giving ones" they have been active in the hang gliding community CBCC & USHPA for 30+ years, always there to donate time and money for various needs in our flying community. They also donate their time to their whippet club WWWA. Now it's time for us to help them with their fight to recover from breast cancer. Kerie will have on going thearapy and reconstruction surgery this May. She plans her first hang gliding flights after reconstruction surgery will be this summer in Chelan, WA. After the masectomy last year her first flights were also in Chelan where she reached 10,000ft! So that is our goal for this fund raising site, I would love it to be more if possible to help with travel to medical appts. and house keeping help if possible. Please donate what you can and share this to all your friends and family!
Below is a more detailed account of Kerie's adventure with breast cancer that was written by her husband. I had asked him to write about how they have dealt with it so far so that I could share it with other patients (I'm sneaky like that.) -Tina Jorgensen
Kerie's Story (by Aaron Swepston)
Kerie had just recently had her annual exam where her doctor performed a standard manual exam of her breasts and found to her satisfaction that they felt normal. She was also supposed to schedule a mamogram, and she planned on doing that within a few weeks, but with the regular exam appearing normal it was easy to relax about scheduling that appointment.
A couple of weeks later, she noticed a lump in her right breast, which for many women is not completely unusual. Lumps can come and go as a part of some women’s normal cycles, but this one was unusual in that it was slightly painful when manipulated. Concerned, she asked me to take a look at it to see what he could feel and what he thought. Yes, it was a definite lump, and it was the fact that it was a bit painful when located, manipulated or pressed that produced some red flags. Since she was supposed to schedule a mamogram soon, this was all the more reason to schedule it as quickly as possible and point out the lump for more specific examination. A lump that was missed by a doctor’s examination, yet discovered during a casual self examination. That was how it all began.
The mamogram was scheduled, and during the exam the lump was more closely examined. The lump was definitely an area of concern, showing some speckles or granulation, and a biopsy followed. It would take a bit of time to get the results of the biopsy back, and we were leaving on a vacation to California for a week. The second day into our trip, as we were nearly Santa Rosa as our jump off point for doing some wine tasting tours, we got the call. There are always these calls and those calls, all sorts of calls that you receive, some from your doctors even. But this was THE call, the one where they ask you what you are doing, whether you are driving or not, if you are okay; basically making sure that you are in a position to handle the news that they are going to give you and not “lose it” such that you run off the road and crash, or fall down in a store somewhere out of shock. She said she was fine, she was on the road but not the one driving, so yes, please let me know what is up. The caller on the other end was as kind as possible, but the gist of the next sentence went something along the lines of “We have the biopsy results back, and you have cancer.” Kind of just like that.
Sometimes I’m really good at telling time, and sometimes I’m a bit off, but for the life of me I can’t remember whether we were half an hour out of Santa Rosa, or 45 minutes, or an hour. I just know that following that call, we were each immersed in our own rambling thoughts, and were engaged in talking about them in as positive a way as possible. But part of that call had indicated that while it was not extremely urgent to get back for treatment, that this was an unusually aggressive form of cancer and we want to get on it as quickly as possible. So, to keep from slipping into excessive fear, worry, depression and so on, we spent part of the remaining drive calling the various doctors’ numbers and trying to get appointments set up as quickly as possible so we could get on the books, waste no time, and not have anything hanging over our heads as not yet done. After a bit, appointments were in the works, we’d hear more soon, details would be worked out and so we had done all that we could do in terms of getting the medical plans geared up to go. Then comes the calls back home. To family. Those are hard calls to make. Knowing one has cancer, but being relatively ignorant about what that means, and not having additional information to answer the inevitable questions. Being in the dark is a terrible place to be when all you really know is that you have cancer, and it is aggressive, and let’s get you going with a treatment plan. Which you will be told about later. Everything is later.
With the doctor calls taken care of, and the family calls made, we roll into Santa Rosa, park the RV, and say to ourselves, “time to go wine tasting, and I am not spitting any of it out!” Thinking back, it was probably one of the best places we could have gotten the news. It would be easy to think otherwise, but the fact is, we were in a beautiful part of the country, wineries, mountains, beautiful views, apart from the workaday world, on vacation, where you can really look around and appreciate the life that you have. The wine tasting occupies time and thoughts, the driving in between is refreshing and distracting. There’s probably never a good time or place to get news like this, but all in all I think it was probably one of the better options. It was a good vacation, while it lasted.
Once getting home, we hit the ground running. Our first appointments were with a surgeon, and she talked to us about options that she thought were likely. She was extremely nice, and very likable, but with cancer one has to also use an oncologist, the doctor that deals with the medical side of the disease. The surgeon deals with the surgical side while the oncologist deals with the disease itself. We were already starting to learn. We were scheduled to see an oncologist in the same facility, and when looking him up online that evening, we were starting to get other options via friends and family, and eventually Kerie’s primary doctor called and said in no uncertain terms that she would need to see a specific oncologist, a trusted friend of hers, and that was that. So we called her, and were told that we might be able to get in depending on what Kerie’s chart looked like. Might be soon, might not be, who knows. We received a cal saying come in right away, she would see us after hours, and again, that was that. The oncologist’s name is Sibel Blau. She is a hero. She has a passion for her work that is amazing, and her dedication to her patients is outstanding.
The biology and pathology and genetic makeup of this particular cancer determined chemo treatment in advance of surgery, there would be this sort of treatment, that sort of treatment and a whirlwind of medical testing, analysis, and treatment. And we were well informed at every point along the way. The treatment plan was specifically targeted towards Kerie’s specific and unique form of cancer, and it started with the placement of a “port”, a sort of artificial vein that is installed in the upper chest that is accessible for intravenous injections and drip medicines, where a small disk shaped device serves as the target for the needles. Finding a good vein, and sticking a needle in it over and over again is not the best way to go, it scars veins, is hard on the nurses and the patients, so a port is a wonderful way to get medicines into the bloodstream. Just poke a needle through the skin, hit a dime sized target in the device, and the medicines flow through it, up a tube that has been inserted into a major vein in the neck. One surgery to install that port, and getting hooked up for weekly chemo treatments becomes as simple as a skin prick. At least in terms of administering the drugs. Then there are the drugs.
Some chemo drugs are generalized, intended to kill a wide variety of cancer cells. And some are more specific, targeted very precisely to the genetic structure of one’s own cancer cells. All cancer cells are not alike. In fact, few are actually alike, which makes it difficult to treat cancer with a one cure for all sort of plan. Kerie’s cancer was estrogen positive, which means that estrogen, the female hormone, stimulated its growth. The bad part of that is that to fight Kerie’s cancer, they needed to subdue her estrogen. That means menopause. Welcome to menopause and all the wonderful things that go along with that! The good part, however, is that because her cancer had estrogen receptors, cellular parts that would allow estrogen in as a sort of growth factor, they could use drugs that would penetrate those estrogen receptors and disable the cancer cells. These cancer cells feed on estrogen, so give them something that tastes like estrogen to them and they choke on it! At any rate, this is the sort of targeting that the oncologists can do with cancers, they can specifically tailor their chemo treatment to specific types of cancers. While Kerie’s cancer was an aggressive form, it was vulnerable to certain types of chemo treatment.
A couple weeks after starting chemo treatment, Kerie’s hair started falling out. We knew when it would happen, the doctors told us it happens on a fairly exact schedule. They were right. Planning for that, we cut her long, straight, blonde hair off in small ponytails. We would save those and use them to make a sort of wig that she could wear when she missed her long hair. We gave her a snappy short hair cut, and then it started falling out more, and so we cut it shorter, then shorter, then had to buzz it off completely because what was worse than being bald was the hair falling out in clumps and not being able to be washed off very well in the shower. Bald is beautiful, but that partial bald, patchy, nuclear fallout look is far from stylish. And looking less than stylish while undergoing physically and mentally depressing chemo treatment is not fun by any means. Kerie handled it all in stride, for the most part. It’s one thing to be stoic and strong and resilient in everyone’s eyes, and it’s one thing to not give in to the burden of a disease like this, to not be labeled or defined by it, and yet another to actually have to go through it all.
Everyone deals with this sort of thing differently. From the beginning, Kerie didn’t want to be defined by cancer. She did not want to be a cancer patient, a cancer victim, nor a cancer survivor. She didn’t want to have cancer attached to her identity in any way, shape or form. Of course, it’s hard not to be identified as a cancer patient when you have no hair, no eyelashes, no eyebrows, are tired a good amount of the time, are having to go to appointment after appointment, being poked and prodded and cut on and injected and everything else that one has to live with. It’s hard not to become the disease that you want no part of. Kerie never wore the pink hats, the ribbons, the floppy scarf hats that immediately tell everyone from a hundred yards away that you are a cancer patient. Of course she did need to wear hats, just like all bald people need to do in the middle of the winter! But hers were snappy, stylish, and hip. And she looked SO great with no hair. What a perfectly shaped head! But she wasn’t a fan of being bald, she did not use it as a badge of courage or as a sign of her affliction, it was something to deal with as little as possible and move on.
Throughout the chemo treatments, we tried to live as normally as possible. There were times when she felt good enough and strong enough that she could fly, and she did. At other times, she didn’t feel up to it, but managed to maintain as normal a life as possible. She worked the entire time, with the exception of the very beginning of chemo, and during the times directly following surgeries. She was up beat, motivated, and an inspiration. She was the star patient for her oncologist, and was used as an example for other patients as well, showing that life can go on, life can be good, and life can be extremely fun all the while that treatment is going on.
And of course there are the surgeries. First the port placement, along with the biopsies. And then the inevitable, the mastectomies. The breasts have got to go. No way around it, they try to kill you, you cut them no slack. I won’t go into details about that surgery, except to say that it is not a pleasant surgery, it’s not a particularly clean surgery, and it’s not a particularly rosy period of recovery from it. A mastectomy is serious surgery, a lot of tissue is removed, permanently altering one’s body and mental self image. Even though it is considered surgery, the surgical sites are severely damaged and have to drain, repair themselves, and heal. It’s a serious surgery and takes a long time to heal. And depending on whether a woman wants to look relatively normal shaped afterwards or not, various degrees of reconstruction are available. One will never be the same afterwards, but one can achieve a more normal appearance to most people. Some people prefer to have reconstruction, some prefer not, and that’s a very personal decision based on any number of considerations. If one prefers reconstruction, then that comes later, after all other treatments are finished.
In Kerie’s case, she needed to undergo a course of radiation therapy. That is roughly 6 1/2 weeks of daily radiation treatments. Different people respond differently to radiation treatments, but overall the main effects are tiredness, fatigue, and radiation burns in the affected areas. Sort of like a bad sunburn that just gets worse and worse as time goes on. But hey, an additional 20% reduction in the likelihood of recurrence is well worth it. The idea with cancer treatment is to eradicate it completely so that it never comes back. This is something nobody wants to go through once, mush less twice.
So for Kerie, the chemo treatments were followed by a double mastectomy, which was the removal of both breasts. Tissue expanders were put in place at that time because she planned to have reconstruction. That surgery had to heal for six weeks before she could get back to full physical activity. Then another period of time before the radiation could begin, then another six and a half weeks of that. Once that was complete, then another 7-9 months before reconstruction surgery can be done to allow for the radiated tissues to recover as much as they can. The radiated tissues will never recover fully, however. Such is life, such is the price for life. Not such a heavy price to pay. Where we are at the moment is about a month away from the reconstruction surgery, the final medical ordeal to go through before we can put the cancer treatment behind us, hopefully forever.
What is an interesting postscript to all of this is that the loss of hair during the chemo treatment has been replaced with an unexpectedly thick head of extremely curly locks! For some reason, some people’s hair comes back differently than it originally was. While it may change back to pre-chemo straightness at some point, for now Kerie is learning how to deal with an incredibly curly head of hair. How does one deal with hair that will not lay down, will not behave, will not listen to one’s requests or demands that it take some desired shape or form. It’s nice that taming Kerie's crazy, curly hair is is one of the lingering issues to have to deal with now days. It’s kind of a fun new normal. :-)
Below is a more detailed account of Kerie's adventure with breast cancer that was written by her husband. I had asked him to write about how they have dealt with it so far so that I could share it with other patients (I'm sneaky like that.) -Tina Jorgensen
Kerie's Story (by Aaron Swepston)
Kerie had just recently had her annual exam where her doctor performed a standard manual exam of her breasts and found to her satisfaction that they felt normal. She was also supposed to schedule a mamogram, and she planned on doing that within a few weeks, but with the regular exam appearing normal it was easy to relax about scheduling that appointment.
A couple of weeks later, she noticed a lump in her right breast, which for many women is not completely unusual. Lumps can come and go as a part of some women’s normal cycles, but this one was unusual in that it was slightly painful when manipulated. Concerned, she asked me to take a look at it to see what he could feel and what he thought. Yes, it was a definite lump, and it was the fact that it was a bit painful when located, manipulated or pressed that produced some red flags. Since she was supposed to schedule a mamogram soon, this was all the more reason to schedule it as quickly as possible and point out the lump for more specific examination. A lump that was missed by a doctor’s examination, yet discovered during a casual self examination. That was how it all began.
The mamogram was scheduled, and during the exam the lump was more closely examined. The lump was definitely an area of concern, showing some speckles or granulation, and a biopsy followed. It would take a bit of time to get the results of the biopsy back, and we were leaving on a vacation to California for a week. The second day into our trip, as we were nearly Santa Rosa as our jump off point for doing some wine tasting tours, we got the call. There are always these calls and those calls, all sorts of calls that you receive, some from your doctors even. But this was THE call, the one where they ask you what you are doing, whether you are driving or not, if you are okay; basically making sure that you are in a position to handle the news that they are going to give you and not “lose it” such that you run off the road and crash, or fall down in a store somewhere out of shock. She said she was fine, she was on the road but not the one driving, so yes, please let me know what is up. The caller on the other end was as kind as possible, but the gist of the next sentence went something along the lines of “We have the biopsy results back, and you have cancer.” Kind of just like that.
Sometimes I’m really good at telling time, and sometimes I’m a bit off, but for the life of me I can’t remember whether we were half an hour out of Santa Rosa, or 45 minutes, or an hour. I just know that following that call, we were each immersed in our own rambling thoughts, and were engaged in talking about them in as positive a way as possible. But part of that call had indicated that while it was not extremely urgent to get back for treatment, that this was an unusually aggressive form of cancer and we want to get on it as quickly as possible. So, to keep from slipping into excessive fear, worry, depression and so on, we spent part of the remaining drive calling the various doctors’ numbers and trying to get appointments set up as quickly as possible so we could get on the books, waste no time, and not have anything hanging over our heads as not yet done. After a bit, appointments were in the works, we’d hear more soon, details would be worked out and so we had done all that we could do in terms of getting the medical plans geared up to go. Then comes the calls back home. To family. Those are hard calls to make. Knowing one has cancer, but being relatively ignorant about what that means, and not having additional information to answer the inevitable questions. Being in the dark is a terrible place to be when all you really know is that you have cancer, and it is aggressive, and let’s get you going with a treatment plan. Which you will be told about later. Everything is later.
With the doctor calls taken care of, and the family calls made, we roll into Santa Rosa, park the RV, and say to ourselves, “time to go wine tasting, and I am not spitting any of it out!” Thinking back, it was probably one of the best places we could have gotten the news. It would be easy to think otherwise, but the fact is, we were in a beautiful part of the country, wineries, mountains, beautiful views, apart from the workaday world, on vacation, where you can really look around and appreciate the life that you have. The wine tasting occupies time and thoughts, the driving in between is refreshing and distracting. There’s probably never a good time or place to get news like this, but all in all I think it was probably one of the better options. It was a good vacation, while it lasted.
Once getting home, we hit the ground running. Our first appointments were with a surgeon, and she talked to us about options that she thought were likely. She was extremely nice, and very likable, but with cancer one has to also use an oncologist, the doctor that deals with the medical side of the disease. The surgeon deals with the surgical side while the oncologist deals with the disease itself. We were already starting to learn. We were scheduled to see an oncologist in the same facility, and when looking him up online that evening, we were starting to get other options via friends and family, and eventually Kerie’s primary doctor called and said in no uncertain terms that she would need to see a specific oncologist, a trusted friend of hers, and that was that. So we called her, and were told that we might be able to get in depending on what Kerie’s chart looked like. Might be soon, might not be, who knows. We received a cal saying come in right away, she would see us after hours, and again, that was that. The oncologist’s name is Sibel Blau. She is a hero. She has a passion for her work that is amazing, and her dedication to her patients is outstanding.
The biology and pathology and genetic makeup of this particular cancer determined chemo treatment in advance of surgery, there would be this sort of treatment, that sort of treatment and a whirlwind of medical testing, analysis, and treatment. And we were well informed at every point along the way. The treatment plan was specifically targeted towards Kerie’s specific and unique form of cancer, and it started with the placement of a “port”, a sort of artificial vein that is installed in the upper chest that is accessible for intravenous injections and drip medicines, where a small disk shaped device serves as the target for the needles. Finding a good vein, and sticking a needle in it over and over again is not the best way to go, it scars veins, is hard on the nurses and the patients, so a port is a wonderful way to get medicines into the bloodstream. Just poke a needle through the skin, hit a dime sized target in the device, and the medicines flow through it, up a tube that has been inserted into a major vein in the neck. One surgery to install that port, and getting hooked up for weekly chemo treatments becomes as simple as a skin prick. At least in terms of administering the drugs. Then there are the drugs.
Some chemo drugs are generalized, intended to kill a wide variety of cancer cells. And some are more specific, targeted very precisely to the genetic structure of one’s own cancer cells. All cancer cells are not alike. In fact, few are actually alike, which makes it difficult to treat cancer with a one cure for all sort of plan. Kerie’s cancer was estrogen positive, which means that estrogen, the female hormone, stimulated its growth. The bad part of that is that to fight Kerie’s cancer, they needed to subdue her estrogen. That means menopause. Welcome to menopause and all the wonderful things that go along with that! The good part, however, is that because her cancer had estrogen receptors, cellular parts that would allow estrogen in as a sort of growth factor, they could use drugs that would penetrate those estrogen receptors and disable the cancer cells. These cancer cells feed on estrogen, so give them something that tastes like estrogen to them and they choke on it! At any rate, this is the sort of targeting that the oncologists can do with cancers, they can specifically tailor their chemo treatment to specific types of cancers. While Kerie’s cancer was an aggressive form, it was vulnerable to certain types of chemo treatment.
A couple weeks after starting chemo treatment, Kerie’s hair started falling out. We knew when it would happen, the doctors told us it happens on a fairly exact schedule. They were right. Planning for that, we cut her long, straight, blonde hair off in small ponytails. We would save those and use them to make a sort of wig that she could wear when she missed her long hair. We gave her a snappy short hair cut, and then it started falling out more, and so we cut it shorter, then shorter, then had to buzz it off completely because what was worse than being bald was the hair falling out in clumps and not being able to be washed off very well in the shower. Bald is beautiful, but that partial bald, patchy, nuclear fallout look is far from stylish. And looking less than stylish while undergoing physically and mentally depressing chemo treatment is not fun by any means. Kerie handled it all in stride, for the most part. It’s one thing to be stoic and strong and resilient in everyone’s eyes, and it’s one thing to not give in to the burden of a disease like this, to not be labeled or defined by it, and yet another to actually have to go through it all.
Everyone deals with this sort of thing differently. From the beginning, Kerie didn’t want to be defined by cancer. She did not want to be a cancer patient, a cancer victim, nor a cancer survivor. She didn’t want to have cancer attached to her identity in any way, shape or form. Of course, it’s hard not to be identified as a cancer patient when you have no hair, no eyelashes, no eyebrows, are tired a good amount of the time, are having to go to appointment after appointment, being poked and prodded and cut on and injected and everything else that one has to live with. It’s hard not to become the disease that you want no part of. Kerie never wore the pink hats, the ribbons, the floppy scarf hats that immediately tell everyone from a hundred yards away that you are a cancer patient. Of course she did need to wear hats, just like all bald people need to do in the middle of the winter! But hers were snappy, stylish, and hip. And she looked SO great with no hair. What a perfectly shaped head! But she wasn’t a fan of being bald, she did not use it as a badge of courage or as a sign of her affliction, it was something to deal with as little as possible and move on.
Throughout the chemo treatments, we tried to live as normally as possible. There were times when she felt good enough and strong enough that she could fly, and she did. At other times, she didn’t feel up to it, but managed to maintain as normal a life as possible. She worked the entire time, with the exception of the very beginning of chemo, and during the times directly following surgeries. She was up beat, motivated, and an inspiration. She was the star patient for her oncologist, and was used as an example for other patients as well, showing that life can go on, life can be good, and life can be extremely fun all the while that treatment is going on.
And of course there are the surgeries. First the port placement, along with the biopsies. And then the inevitable, the mastectomies. The breasts have got to go. No way around it, they try to kill you, you cut them no slack. I won’t go into details about that surgery, except to say that it is not a pleasant surgery, it’s not a particularly clean surgery, and it’s not a particularly rosy period of recovery from it. A mastectomy is serious surgery, a lot of tissue is removed, permanently altering one’s body and mental self image. Even though it is considered surgery, the surgical sites are severely damaged and have to drain, repair themselves, and heal. It’s a serious surgery and takes a long time to heal. And depending on whether a woman wants to look relatively normal shaped afterwards or not, various degrees of reconstruction are available. One will never be the same afterwards, but one can achieve a more normal appearance to most people. Some people prefer to have reconstruction, some prefer not, and that’s a very personal decision based on any number of considerations. If one prefers reconstruction, then that comes later, after all other treatments are finished.
In Kerie’s case, she needed to undergo a course of radiation therapy. That is roughly 6 1/2 weeks of daily radiation treatments. Different people respond differently to radiation treatments, but overall the main effects are tiredness, fatigue, and radiation burns in the affected areas. Sort of like a bad sunburn that just gets worse and worse as time goes on. But hey, an additional 20% reduction in the likelihood of recurrence is well worth it. The idea with cancer treatment is to eradicate it completely so that it never comes back. This is something nobody wants to go through once, mush less twice.
So for Kerie, the chemo treatments were followed by a double mastectomy, which was the removal of both breasts. Tissue expanders were put in place at that time because she planned to have reconstruction. That surgery had to heal for six weeks before she could get back to full physical activity. Then another period of time before the radiation could begin, then another six and a half weeks of that. Once that was complete, then another 7-9 months before reconstruction surgery can be done to allow for the radiated tissues to recover as much as they can. The radiated tissues will never recover fully, however. Such is life, such is the price for life. Not such a heavy price to pay. Where we are at the moment is about a month away from the reconstruction surgery, the final medical ordeal to go through before we can put the cancer treatment behind us, hopefully forever.
What is an interesting postscript to all of this is that the loss of hair during the chemo treatment has been replaced with an unexpectedly thick head of extremely curly locks! For some reason, some people’s hair comes back differently than it originally was. While it may change back to pre-chemo straightness at some point, for now Kerie is learning how to deal with an incredibly curly head of hair. How does one deal with hair that will not lay down, will not behave, will not listen to one’s requests or demands that it take some desired shape or form. It’s nice that taming Kerie's crazy, curly hair is is one of the lingering issues to have to deal with now days. It’s kind of a fun new normal. :-)
Organizer and beneficiary
Tina Jorgensen
Organizer
Spanaway, WA
Aaron Swepston
Beneficiary