
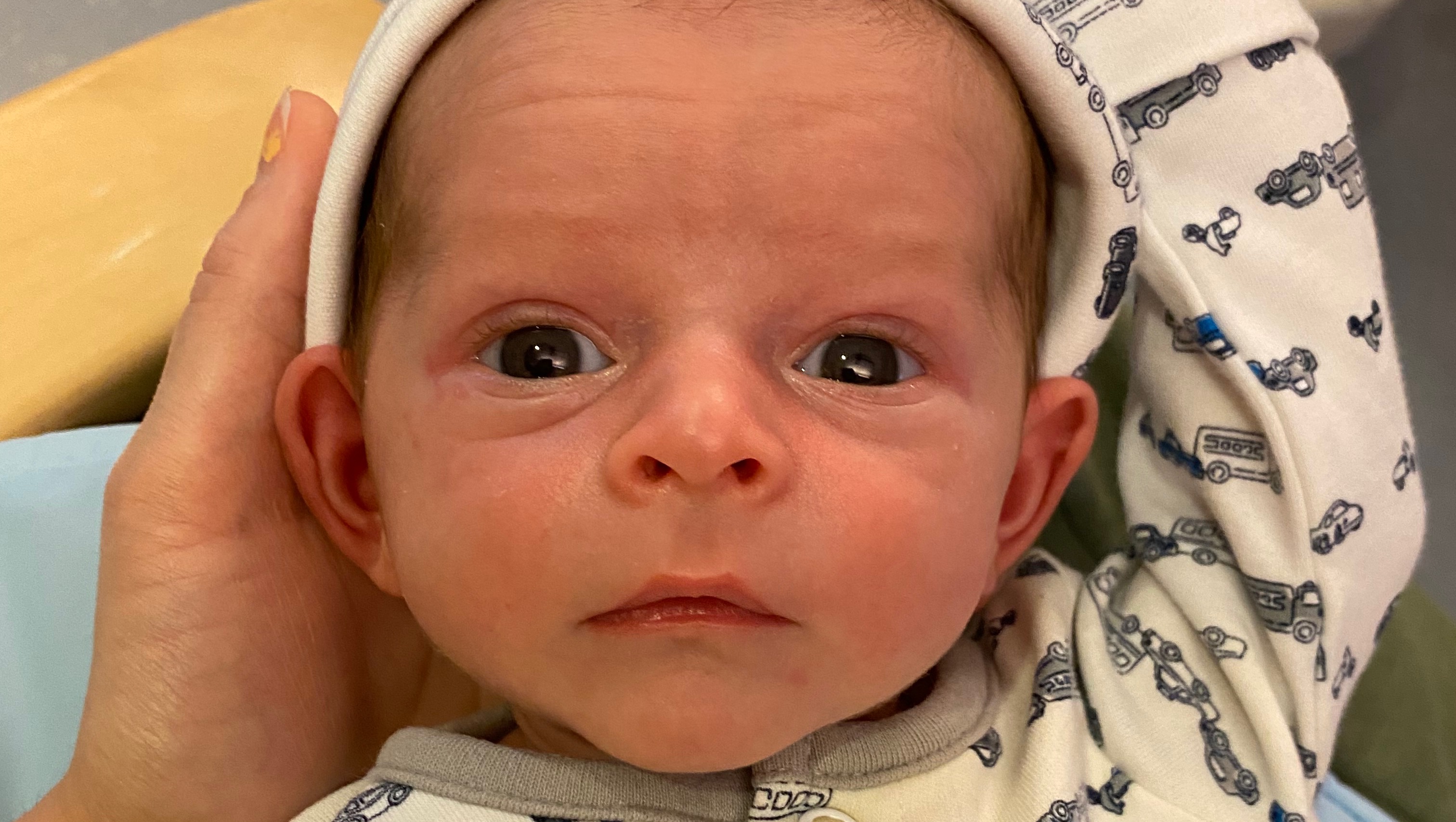
Our first family picture welcoming our baby boy into the world looks like so many others. LeRoy Andrew was born on 10/24/2021 early in the morning, and was presumed healthy after a turbulent VBA2C delivery. He is the third child in our immediate family with an older sister (Adelaide, 7 years), and an older brother (Walker, 4 years) who were so excited to learn wether he would be a boy or girl. Since he was our third baby we joked the entire time that he would be our “mystery tie-breaker!” Little did we know what a mystery he would be truly bringing us.
The first 24 hours with LeRoy at the hospital were fairly normal, however Matthew and I had some concerns surrounding minor peculiar behaviors we noticed our first night together. LeRoy seemed to eat very well, but spit up quite profusely despite burping successfully after feeds no matter what we would do. He also shook and shuddered as he breathed in his sleep. When we brought up our concerns they were considered within the realm of normal by nursing staff and we did our best to brush off the concern. After all we had a healthy and (mostly) uneventful pregnancy and delivery.. Aside from my hemorrhaging and complex repair at least. By the next morning we were prepared to be discharged and bring home our sweet little surprise bundle home to let big brother and sister know just exactly who would be joining our family.
Our nurse for the morning started with the typical newborn screenings all babies get before being sent home, starting with measuring his 02 sats, or in other words, Oxygen levels. His initial reading was in the 70’s, where a normal healthy baby should be at 100 or at least not below 95. Because he looked good otherwise she thought it may have been a number of things; cold feet, a faulty machine or hookup, etc. She tried everything from rolling in a new monitor, adjusting the pulse oximeter on each foot as well as his wrists, to even warming his appendages with small heat packs, but nothing was budging that number. She consulted with our medical team who all genuinely believed he was mostly well but may have still had residual fluid in his lungs from delivery or that it was some sort of fluke. We were asked if he could go into an hour of “observation”, to which we both happily agreed using that time to rest up ourselves. After all I had labored and delivered with no pain medicine or medical intervention and was quite tired, as was Matthew after being my support person.
After the hour of observation LeRoy was unfortunately not making much progress, even while being given supplemental oxygen via cannula’s (the oxygen tubes that go in the nostrils). We were invited to go see him as they drew blood work and prepared to move him to their NICU for imaging and closer observation. That alone was a scary adjustment but we had no idea how turbulent our next few weeks would be. His x-rays did show a small amount of fluid on the lungs which was the initial suspected diagnosis, I was allowed to continue nursing him and we stayed in the NICU keeping a close watch on our sweet boy.
At this point despite supplemental oxygen his O2 sats were not where they should have been. The medical team recommend he be evaluated at some point by a cardiologist in an abundance of caution. After all there are only a few very rare cardiovascular disorders that are not caught in-utero, and our pregnancy was healthy at all regular ultrasounds and Doppler checks. There was a cardiologist coming to see another baby who was much more ill than LeRoy, but she decided to make time to evaluate him as well. She later said she “just had a hunch” that she should look at his heart while already there. We are so grateful for this happening. We stood with her as she did the scan, and after about an hour we asked how many pictures she generally takes for an echocardiogram. Her response was, “anywhere from 100-120”… She was on frame 179. My heart sank as I looked at Matthew and we made that eye contact that so many of us know, sheer uncertainty tainted with a fresh level of parental worry. She was soon finished and we were left with so many unanswerable questions that would have to wait until his images were evaluated.
Matthew left LeRoy and I at the hospital so he could take home some of our belongings to exchange, and so that he could grab a bite to eat. We were well aware at this point that we would not be leaving the hospital with our newborn son anytime soon. After a quick trip through a drive thru he arrived at our apartment and gave the kids and his Mom, who was phenomenally there to help, a brief rundown of the situation. I continued to hold LeRoy and nursed him trying to keep him comfortable as much as possible. While Matthew was gone I met the second cardiologist working on LeRoys case who told me “there were some concerns” on his echo screening and that they were sharing his images with colleagues both in house and out of house.
My concern grew steady as I waited patiently both for Matthew to return and for the final verdict on LeRoys readings. Not too long had passed, though I don’t exactly know how much or little time it was exactly, before the original cardiologist came back and asked me if she could sit with me to talk. This was terrifying. I felt like life moved into freezeframes or stop motion photography from an old medical film. My heart sank as I felt the seriousness and urgency in her tone and the NICU nurse closed the curtains around our small corner of the room.
My memory surrounding this conversation is still somewhat hazy as I was absolutely overwhelmed with emotions in these moments. She told me that his images were “quite concerning” along with a brief explanation of how disproportionate the chambers and pressures within his heart were. She had sent images to UCSF Benniofs Childrens Hospital, and they wanted him there immediately. He needed heart surgery, a bypass open heart surgery. His life was at great risk and he would not likely survive without immediate operative correction, though he did not yet have a diagnosis. My vision went darker and I felt hot tears swelling in my eyes, my body shook as I held and nursed our new son. He was less that 30 hours old. He needed to be transported via helicopter and to keep him medically stable he needed to start a medication called “PGE” which in turn required him to be intubated. I was asked to stop nursing him in these moments. She even offered to take pictures of me holding him before he was intubated. I obliged in an abundance of fear and prepared myself to call my husband and try to coherently and urgently communicate to him both to hurry back, and an overview of LeRoys condition.

I had no idea how long it would be, or if I would ever get to hold LeRoy again. I sat in my chair feeling completely surrounded and entirely alone at the same time, waiting for helicopter transport to show up and waiting on paperwork to release our son. It took less than an hour for him to be intubated and for the transport team to show up. That hour took both forever and no time at all. Matthew got back to the hospital just before the transport team did and he was able to say a brief goodbye to LeRoy as we prepared to ask for an early discharge for myself. I was not feeling great having waves of nausea and dizziness but chalked it up to the stress of the situation. I was using a wheelchair for long walks but hobbled around the room gathering anything I could and waited to speak to my nurse after mentioning to the desk that I needed to go. As our son was life flighted to UCSF, I picked up the package of diapers I didn’t know if I would ever get to put on him. I cried, I worried if his flight would make it in time and if he did, would we make it from Roseville to San Francisco in time?
My nurse came in more than ready to accommodate the request for early discharge, and offered any help she could give. We rushed everything. Our packing and loading of the room and our car, signing paperwork, preparing ourselves for the journey. It was 11:00 PM when we got back to our apartment to say our goodbyes to our sleeping children. Adelaide and Walker were sleeping so hard we didn’t get hugs but instead gave kisses and whispers of love and reassurance to them. I packed us peanut butter and jelly sandwiches, and we ate them in the car for dinner. They were awful and tasted like grief.
Mathew’s older brother and sister in law, Tim and Lorie, live close to San Francisco and offered to see LeRoys flight land at the childrens hospital. As we rushed as safely as possible there, we were receiving photos and texts of the helicopter landing and the transport team rolling him into the hospital from the roof.

It was both relieving and a whole new weight to carry knowing we were moving closer to our infants open heart surgery, hoping for a more pointed diagnosis. When we eventually got there, there was a pediatric cardiologist assigned to our case who we were told to wait for. It was 1:00AM. I was exhausted and faint even sitting in my wheelchair and Matthew kept asking if I was okay, all I could answer was “I don’t know.”
Soon the pediatric cardiologist came to sit and talk with us. We had both been crying in a room filled with notes of encouragement and donations of knit hats for babies and baby blankets, pamphlets on navigating grief, and tons of information on the many diseases the hospital treats in children. He gave us a rundown of their plans to diagnose and stabilize our son, all of which we agreed to and signed the necessary paperwork for. He then turned directly to me and expressed concern for my present state. Apparently I looked as bad (or worse) than I felt, he recommended I be evaluated by their Labor & Delivery department. Matthew wheeled me into triage where I received blood work panels and was left alone in a quiet room to rest while he went upstairs to see LeRoy. By 3:00AM my blood work showed extremely low values on my CBC and I was given a room in L&D, as well as a blood transfusion and an iron drip. Soon after I was updated that Matthew followed LeRoy to his room in the Cardiac Intensive Care unit and was also able to get some sleep himself. LeRoy received additional blood work, another EKG and echocardiogram, and we continued to wait and began praying heftily.
The next 24 hours was highly educational, as LeRoy was given an official diagnosis of TAPVR Infra-cardiac with mixed veins, as well as ASD. (These acronyms stand for; Total Anomalous Pulmonary Venous Return, and Atrial Septal Defect). They were concerned, however, that LeRoy might also have an infection as he had a slight fever and his blood cultures from the NICU in Roseville showed growth. He was assigned a whole team as each child at UCSF is, and we were told his surgery would be delayed as we established wether it not he was additionally battling an infection. It took 4 long and painful days to rule out infection but by that point we were so grateful that we could move forward with the surgery that would hopefully save his life.
We stayed with Family House, an utterly stunning organization that houses the families and children seeking medical treatment of life threatening diseases at UCSF. They also provide assistance with meals, and support for siblings when needed. We took the journey to UCSF daily and stayed as much with LeRoy as we could to simply be with him, as well as to show him our love and support while he was there. He was intubated and sedated so all we could do was stroke his hair and hands, read to him, talk and sing to him, and help with his basic care. I was allowed to pump there in his room and they stored milk in hopes post-op he would be able to drink it. The staff was full of beautiful people I will never forget.

He looked so small in a room full of machines, all working to keep him alive. I got to hold him one time in the days we waited for his surgery, and so did Matthew. But the movement sent him into tachycardia and we didn’t want to put him through that stress just for our benefit.


The night of 10/29 (his last night pre-surgery) I gave LeRoy his first hint of being bathed, I washed his hair. I was terrified, but he hadn’t been bathed yet and I really wanted to be a part of that process. The next day as we prepared for surgery it was so turbulent. That morning we were told “The doctor would like to fit LeRoy in today, but we are not sure yet.” A couple hours later during rounds we were told it would likely be Sunday instead. Then another hour after that he was officially on the docket for surgery, as another child had spiked a fever and would be unable to have their surgery. I remember stroking his bare chest, wondering if his scar would hurt him as it healed, and hoping it would get the chance to do so. We prayed over our son, we sat as close as we could while we waited to sign the final round of paperwork giving permission for the procedure to take place, and we held back heavy painful tears of fear and uncertainty. LeRoy had already proven to be a strong soul, but we had no power over the situation and this was the hardest thing either of us have ever gone through as parents or otherwise.
By mid afternoon we followed the team and our son from the CICU, to as far as we could go towards the OR. We kissed our son and left the hospital to wait for the news of the surgery finishing, for better or for worse. We ate sushi. Sushi was the meal I thought would be our celebratory victory meal and possibly our first family outing once we brought our new baby home. We cried in a public restaurant and ate very little, but we gave our best effort at nourishing our bodies knowing this was really just the start of a long journey with our sons diagnosis. We sent a lot of texts and waited anxiously for the call that he was done and hopefully alive. When the time finally came, it was a whole new level of relief and excitement much different either of us had ever felt. We rushed back to the hospital and met the miracle surgeon who performed the correction on LeRoy, his name is Dr. Reddy. He humbly educated us on the success of the operation, shying away from our compliments and unbridled gratitude before rushing off to literally save more lives. I was so weak and tired at this point, but tried so hard to persevere and make it to see our son back in his room. Tim and Lorie came back to have a very late dinner with us, and we all sat in the UCSF lobby just waiting and talking and enjoying the opportunity to catch up on so much together. I was losing my ability to stay awake and well, as it was just after midnight. Matthew took me back to Family House to rest before going back to wait in the lobby more. I pumped, showered and rested for a short time before getting a call from Matthew that LeRoy was settling in his room. It was the wee hours of the morning and I could not wait to get back there.

Going in to see him early the next morning, he didn’t look real to me. But he was real, and we could see his heart beating. While his chest being opened was somewhat unsettling, I’ve never seen anything more beautiful than his heart functioning normally. I have attached a link at the bottom of the page explaining his TAPVR diagnosis as well as the other types of TAPVR that exist. His was quite complicated and we are so incredibly grateful he endured the surgery and the repair was so successful. This picture was taken early morning 10/30/2021.
We continued our routine of long days at UCSF, and started an email address for friends and family to send words of encouragement to LeRoy and read them to him each day. We read him books, we sang him songs, and we loved him the best we could. His chest was closed on Halloween, and his nurse for daytimes in recovery brought and helped us dress him in his first costume. Something we didn’t think we could do. His nighttime nurse helped too, and we were blessed to have their care for multiple days in a row. They both helped us so much in his care, in answering questions, and in loving our son whenever we had to be away from him.

LeRoy was also exactly 1 week old on Halloween.

The following 2 weeks would be our final weeks in LeRoys original admission to UCSF. During this time he did quite well healing! His siblings got to meet him in the hospital, and his care team navigated his big challenge of tachycardia arrhythmia with medication that seemed to work just as it was needed to.
To keep this already long story slightly more brief than it could be I will share just a few more pictures rom his stay, and conclude this writing with a summary of our needs for financial help with his medical bills.




Since his initial stay at UCSF LeRoy has been on one additional life flight to UCSF after an aspiration caused him to go unconscious and unresponsive in the car. He has also been hospitalized once more locally for suspected infection. We are still waiting for cultures so fully confirm or deny that suspicion. The first life flight alone was $84,000( we are hopeful our insurance will cover a portion, but UCSF is considered “out of network” for us), and we have yet to even see his other medical bills. We are sure we will be paying into these bills for quite a long time, but that’s okay. We just would like some help at least in getting them started as we see them continue to roll in.
Anything and everything helps, including simply sharing our page, words of encouragement, and prayers for LeRoys health moving forward. If you have made it this far in reading, THANK YOU! I hope our story is educational and inspiring for other families battling CHD, and for those who may not even realize that childhood heart disease is a “thing” for some. Less that 1% of children have CHD, and less than 1% of those children have TAPVR Infracardiac. Not too long ago this diagnosis would have been a death sentence and we are so grateful to have the time we have had with LeRoy, and look forward to as much more as we are granted.

Happy Holidays and tons of hope to you and yours this holiday season, and again, thank you!

