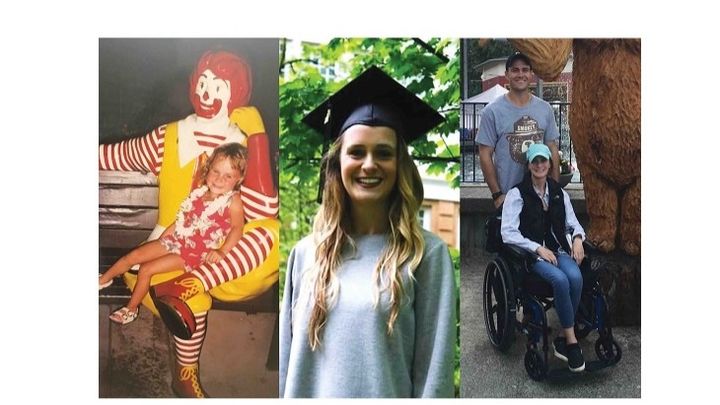
Cause for Breath: Rene's Story
Rene Vania and her family need your help to beat an illness she’s been fighting her entire life. Rene suffers from idiopathic pulmonary fibrosis (IPF), which is a chronic lung disease that generally manifests itself in older patients; however, Rene was born with the condition. It is a lung disease that results in irreversible scarring (fibrosis) of the lungs for an unknown reason. The scarring restricts the amount of oxygen her lungs can take in as the passageways that carry air become narrower over time. Eventually her lungs will not be able to provide enough oxygen for her body to live, and her only option for survival will be to receive a new set of lungs. Unfortunately, that time is NOW...
Rene’s condition has come to a point where her lungs are no longer sustainable and the only option for recovery is to undergo a major life-saving surgery. She now needs a double-lung transplant where she will receive a set of healthy lungs from a donor. There is hope and excitement that Rene may soon breathe deeply and fully for the first time in her life, and for the rest of her life.
I'm Rene's big brother and I started this campaign to help my sister get the funds she needs for her surgery, as well as the many expenses before and after the operation. I don't want her to worry about how to pay for her apartment after being compelled to live in a new city awaiting a lung transplant. I don't want her to worry about the cost of post-operative follow-up and her recovery.
When Rene was born, I was so freaking excited to have a little sister! I even took her to school as my show-and-tell project. Then, just a couple days after her homecoming she was rushed to the emergency room. She spent a month in the hospital as pediatric specialists tried to determine why her breathing was labored and she had become tachycardic (rapid heartbeat). My kindergarten teacher had the whole class write her “get well” cards and everyone became emotionally invested in Rene’s wellbeing. I was such a proud big brother! I was going to protect my sister always.
The initial diagnosis was reflux and a Nissen fundoplication procedure was performed to tighten things up around the esophagus. At about 11 months, the pediatrician diagnosed Rene as failure to thrive. She was only 13 pounds. Another round of testing by the pediatric specialists was started. The GI doctor noticed there was clubbing at the ends of her fingers (which usually means oxygen is not getting pumped to the extremities), so he sent her to the pediatric cardiologist who found her heart to be in good shape. The cardiologist sent her to a pulmonologist. The pediatric pulmonologist found some irregularities in her breathing and wanted to do a lung biopsy. Rene went to Children’s Hospital in Seattle and had her first lung biopsy before she turned a year old. She was soon diagnosed with IPF.
Her failure to thrive was because her body was working so hard to breath and move oxygen throughout her body, she needed to consume a lot more calories than normal. The pediatric pulmonologist explained it was like Rene's body was always running a marathon.
Things that weren’t normal for a small child became normal for our family. There was a period of time when Rene was a toddler that she was hooked up to an IV pole, and I remember having to wheel the stand with the bag of fluids dangling from the top around the house. She had large scars on her back and stomach that you don’t see on small children.
There were lots of surprises and we never really knew what to expect.
Occasionally something would happen that would cause her feeding tube to come completely out of the incision in her stomach, and I distinctly recall helping my parents put it back in one night. I remember gritting my teeth and turning my head away while holding my sister’s tiny legs as her body turned deep blue kicking and screaming. I can’t imagine the panic my parents felt having to deal with something they had never expected to be prepared for. It was scary and I hated seeing my baby sister so upset, but I was always willing to help because we all relied on each other to take care of her.
There were a lot of unusual things that had become the norm because they just became a part of life when Rene was born. The only option was to do what was needed to be done to make her strong.
Rene was put on a heavy dose of prednisone (steroids) to slow down the inflammation in her lungs that was causing the scarring. The steroids made her balloon up and she went from this teeny tiny, fragile-looking little baby to a chubby little red-faced girl. I remember she had big happy cheeks. Once she was weaned off the steroids, she was enrolled in the public school.
And eventually she got stronger.
Rene was not one to be coddled and she became active in several sports growing up, like baton twirling, cheerleading, and gymnastics. Her pediatric pulmonologist was often surprised at the activities she participated in. When she took swim lessons, he advised she would need to breathe more often and couldn't hold her breath as long as the other kids. When she played soccer, he advised she would need to rest more often than the other kids. Her physical limitations became obvious during the few seasons she played soccer. She did indeed tire a lot faster than all of the other kids and running really wore her out.
Cardio activities have always been incredibly difficult for Rene, yet she was determined to excel in the physical activities she was able to do. She competed in all of the sports she liked, and practiced extra. Rene made lots of friends through school and sports and she hung out with lots of kids her age. She was a very social teen who still managed to get good grades.
Our family has been incredibly blessed to see Rene healthy for most of her young life. Rene has always been an active, hardworking young woman. I think we all felt she had beat this lung condition. She had finished college at Portland State University, earning her degree in the school of Public Health with a major in Community Health Education and a minor in Aging Services. She was excited about learning to become a respiratory therapist, and chose to begin a new journey across the country to study at McLennan Community College in Waco, Texas. Medication had helped to manage the scarring in her lungs for many years, suppressing the effects of IPF, and she seemed to be living a fairly normal life… up until a couple of years ago when she developed a chronic cough.
Just before moving to Waco and starting classes she found out that her chronic cough and possible sinus infection were actually symptoms of a significant decrease in her lung capacity. She had already been taking hydroxychloroquine which everyone thought was helping to stave off the scarring in her lungs, but for some unknown reason her lungs were continuing to scar. Our entire family was surprised to learn that Rene needed to start talking to a lung transplant specialist.
She moved to Texas knowing Alaska did not have a transplant facility and Texas had several. Rene made appointments with multiple doctors, including the transplant team at UTSW in Dallas. She continued to be optimistic about her condition. She started school while continuing to work. The doctors gave her some additional specialized medication used for IPF and she started going to a pulmonary rehab program. Still her lung capacity continued to decrease and she continued to become more dependent on supplemental oxygen.
Christmas 2018, Rene flew home to visit family in Anchorage, Alaska. Although she was using a portable oxygen concentrator during the flight she became hypoxic, unexpectedly losing motor functions like the ability to hold her head up, move her arms and legs, and talk. Fortunately fellow passengers and flight attendants were able to use additional oxygen onboard to help Rene regain physical function. The incident was incredibly alarming and a huge wake-up-call to our family. Something was very wrong. Rene’s lungs were at the point of no return.
Despite her poor health, Rene returned to school and work. Less than a month later she needed to begin supplementing her oxygen between classes and was forced to give up most of her shifts at work. She had to make the tough decision that she would not be able to continue with University due to her health. Work also took a toll on her and eventually she had to stop working all together.
Rene decided to move to Everett, Washington just outside of Seattle to be closer to family and near the only regional lung transplant facility in the Pacific Northwest. She’s 25 years old, living in a new city, and has no way of making new friends outside of her transplant support group. She is mostly confined to her apartment where she at least feels lucky to live with her long-time boyfriend, who has stood by her through sickness.
Since February 2019 Rene’s life has been completely consumed with focus on her health. She has been trying to gain enough weight to be eligible for a transplant, yet the need for supplemental oxygen is becoming dire. Doctors have assessed her lung capacity is currently at 25% and steadily decreasing at an alarming rate. It feels like suffocating.
Rene's strength and stamina (endurance) have decreased enough that she can no longer complete basic daily tasks she is used to doing independently. She requires assistance getting to doctors appointments and going to the store because she isn’t strong enough to lift her wheelchair and needs the help of a family member to get around. At home she needs help with meals, laundry and other chores. She makes an effort to keep herself busy without getting tired during the day while receiving supplemental enteral nutrition. She requires a continuous supply of fresh oxygen from full-sized tanks she must have with her at all times. This is something a person over the age of 60 experiences after having lived a long and full life, not a 25-year-old! The things Rene struggles with are things we all probably take for granted. Breathing has got to be the most essential bodily function there is!
Although our family struggled with her condition at infancy, we never imagined Rene would actually be facing a lung transplant and all of the challenges that come with it for the entire family. The stakes are even higher this time around.
A double-lung transplant surgery and all of the complications before and after the operation are incredibly scary. The transplant center requires that Rene have 24-hour caregivers for at least three months post transplant. Her family and friends have committed to taking that on.
We are asking your help in making sure she has enough funding required for the surgery and her post-operative needs.
Rene deserves to be healthy. She deserves the best-case scenario. It’s that or nothing…