
Monica McCune, RN-Post COVID Pneumonia Recovery
Donation protected
Thank you for taking the time to read my story of testing positive for COVID, developing pneumonia, the journey it took me on and now my road to recovery.
I prayed for the past couple days about doing this. I need help financially. I was not prepared for this. Should you want to donate though don't feel comfortable doing so online, please let me know. I can give you my mailing address. I have minimal savings after graduating nursing school. I haven't had a paycheck in 4 weeks, My insurance deductible is $4000. I can only imagine how much my hospital stay is and what portion I will be responsible for.
My insurance had been in effect for two weeks when I got sick. I have short term disability though I was told that I had not been employed for 90 days so I would not qualify. Long term doesn't start until one year of employment. How crazy! I kept calling the short term disability people. Finally, I got a call back two days before getting released that I needed to get my Dr. to fill out some forms that my employer likely agreed to let me file. My Dr. for the past 10 days went off shift before the company called and sent me to paperwork. I would be getting a new Dr. the next day. My nurse paged the Dr. who went off and she came back to the hospital, got the paperwork, took it, filled it out and brought it back in a few hours in her pajamas! How lucky am I! Truly blessed! I received confirmation that the short term people received my paperwork on Sept. 8th though I've heard nothing back yet on the official approval.
Also, because I developed the blood clots which is considered an infectious disease and stayed longer than 14 days in the hospital I may qualify for critical illness pay as well. All of this is still in the air and I am not sure what the end result of the coverage will be. I need help now.
I am able to get around though any and all activity is still difficult, my breathing increases, my heart rate gets into the 160's with just 50 feet of walking and my legs can get painful. I can't stay upright on my feet more than 10 minutes at a time. Sometimes, just talking on the phone takes my breathe away. I am so exhausted physically though mentally can't sleep. COVID brain fog is real. I will be talking and just stop, not even realizing it. I'll forget what I wanted to say or what I was saying. I will continue to do things for myself and push myself to move and continue to get stronger. I will still spend most of the day alone. I have found someone to come in and help me a few hours a day with basics like laundry, dishes, meal prep, just being here while I shower as I still need to keep oxygen on, help walk Kiki since I'm tied to this big O2 machine until I can get my portable unit which my step mom has so generously decided to get for me with the intentions it goes to her once I'm well and she'll have it for down the road should she need it. I included a picture of it, it's $4000 alone though will give me freedom to leave the house up to like 6-8 hours and not have to use oxygen tanks that are combustible and only last me one hour per tank at my current 4 liters. Also, I am unable to drive so the caregiver will be able to take me to doctor appointments, physical therapy, grocery store. etc. instead of having to Uber or call a cab.
I'd like to backtrack to the first picture on May 11, 2021. This is my pinning graduation for my Associates Degree of Nursing where I earned my Registered Nurse! This is a HUGE accomplishment that I'm very proud of! I moved to North Augusta, SC with my boyfriend, Jamal after graduation. I interviewed for a job as a RN in March during my spring break in Augusta, GA at University Hospital. I received the contingent offer a week later pending graduation, passing boards late June. I started work in July 2021 working on a intermediate cardiovascular floor. I was three weeks into orientation and had a pre-planned vacation with Jamal and several friends.. We left on August 5th. I started to not feel so good and by August 13, I just was EXHAUSTED! Upon awakening on August 14, I knew in my heart that I had COVID. We had a two day road trip to get back home. No one else with us on vacation tested positive nor got sick. We stopped in NC to pick up Kiki and I used my sisters bathroom, in and out in like 5 minutes with mask on. She tested positive 5 days later and ended up in hospital with COVID pneumonia also for 9 days so we were able to share the experience together, not that i wish that on anyone. To have each other for support and to know what i was going through. God sure has a sense of humor!
I tested positive on August 17th, x-ray was okay. On August 19th, my oxygen levels were 90-92% and fever 103.7 so I went to the ER. I was given IV fluids and antibiotics via IV and sent home four hours later. Jamal had to go out of town this day I went to ER and I asked him to take Kiki (the dog) with him because I just didn't think I could care for her. He of course didn't hesitate. The next two days are fuzzy as I slept a lot. On August 21st, I went back to the doctor office because I was struggling to breathe. Upon arrival, I went straight back and the Dr. called for an ambulance to come get me. Off I went in ambulance and waited for almost 8 hours in the ER they were so overwhelmed and had no rooms. Once I went back for an x-ray and diagnosed with pneumonia, the process was fast and furious as I was admitted to the COVID unit. Much of the first 5 days are a blur to a certain extent though I didn't think I was going to live. The struggle to learn to not fight to breathe with the high flow oxygen at 15-16 liters set a cascade of anxiety. They had to give me a non re-breather mask on top of the high flow just to get me to stop fighting to breathe. I stayed on that for 3 days. After the high flow came off, I was on non re-breather for few days. Finally, I was changed to a Venturi mask in which they can change one piece and be able to titrate the oxygen flow. It took a few days, though I was able to get down to 12 liters. This was a huge success. Day by day, respiratory would change the one piece and continue to lower my oxygen demands until I made it to 6 liters. With each change, the nights were the hardest when I was tired and my body wanted to sleep, the struggle to breathe would return. I had to take Xanax every night to relax as to not set myself back. I never slept more than 4 hours in a night and would stay wake all day until 11pm the next night. Finally, I moved to a regular nasal cannula at 6 liters and that meant we could slowly titrate to get to 4 liters or less as my lungs could tolerate it. I received IV steroids twice a day to help my lungs heal. I went through 4 IV's and the IV team was the only one who could get access right. The steroids were helping but they ate my veins from the inside out. I was finally getting better, feeling like I would actually leave the hospital when I had a huge setback. I woke up Monday, September 6th about 3 am and I could not walk. I felt like my ankles were in vice grips and were being tightened and ripped off. At shift change, I requested my Dr. be called ASAP and she arrived quickly, assessed me, saw no signs of issue except one small touch and I told her I wanted to punch her the pain was so bad. I had begged her everyday to go home. She walked in the room and said "You know you aren't going home right?" I said "yes because I know I have blood clots, can't be anything else!" She ordered ultrasound and in 30 minutes I was diagnosed with bilateral DVTs ( blood clots). This is not good. I had been on Lovenox injections which are blood thinners. I had an intestinal bleed, they stopped the Lovenox. I wore my SCD's which are compression device that go around your calves, attach to a machine and "squeeze" to keep blood flowing good. Unfortunately, they didn't achieve their job. They had to start the injections again after the diagnosis of blood clots and have to stay 24-48 hours longer now. On September 7th, I was officially transferred off the COVID unit out of isolation to a regular med-surg floor with the most amazing view! On 9/8, I couldn't pass my walk test on 4 liters of oxygen. The blood clot pain was so intense, your body requires more oxygen to circulate the blood from heart to lungs to arms, to legs, back up to heart and lungs, repeat, repeat, repeat. I was good on 6 liters. I was stuck another night. I cried a lot. That day, I dislodged the biggest blood clot from my left nostril and within a minute had a headache because i was getting air through the nasal cannula I had struggled to get. I door dashed a nettie pot from CVS. I flushed my sinuses that night. At midnight, my nurse and I walked the hallways. I was able to maintain my oxygen at 4 liters and not drop below 90% oxygen saturation. I flushed the next morning. I kept speaking it that I would pass my walk test on 9/9! Guess what?! I DID IT! The power of positive words!!! By 9:30 am, the Dr. agreed I could go home! 19 days I spent in the hospital! The process began to get home oxygen before I can leave. Jamal had to handle getting all this with case management helping him along the way. He handled all this after work and came picked me up. I had requested he set me up in the living room to be close to all the areas of the house and not stuck in the bedroom. He has been so good to me through all this though I didn't see it when I was in the hospital. He took amazing care of Kiki. That was huge because she is a demanding little 4 pound dog! I'm getting settled back home a little more each day. The first day home, I had a scare as my O2 tubing got kinked while I was on the toilet and I didn't know until my O2 was at 70%. I called 911. I figured it out in a couple minutes though they still came to check me out. In the process, they provided me a humidifier bottle to put sterile water in which helps with nasal moisture and bloody noses. The plus to that is if the tubing gets kinked, it whistles really loud since they water can't "breathe" through the oxygen tubing. The next night, I woke at 2 am and needed to potty. I made it to the toilet and in the process of turning, my knee gave out and i fell. I tried so hard to get up. I had to holler out for Jamal and he was there in 30 seconds flat. Up he got me, finished my business while he cleaned my floor mess/laundry and got me back to bed. By now, I'm thinking that he's thinking I should have not come home yet. This is where this comes into play. Jamal is going into a season at work where he will be working +/- 21 days straight with a wake up time of 2:30 am and won't get home until 7 pm or so. I need help to come into the home with me. It's just him and I here.
This experience has changed me for the better. I can't explain it. I know God has given me this test to become my testimony. This will help me be a better nurse for my patients. I would do it all over again. This is my calling. I can't wait to return to work! I see such huge successes ahead! Once I am recovered and get a good 6 months of work under my belt, I am going back to school for my Bachelors Degree. From there, I see a NP (Nurse Practitioner) degree! My future is so bright! I can't wait! And I promise on all that I am and will be that I WILL PAY IT FORWARD! Thank you!

ADN Pinning Ceremony May 2021

My all in one area in the living room
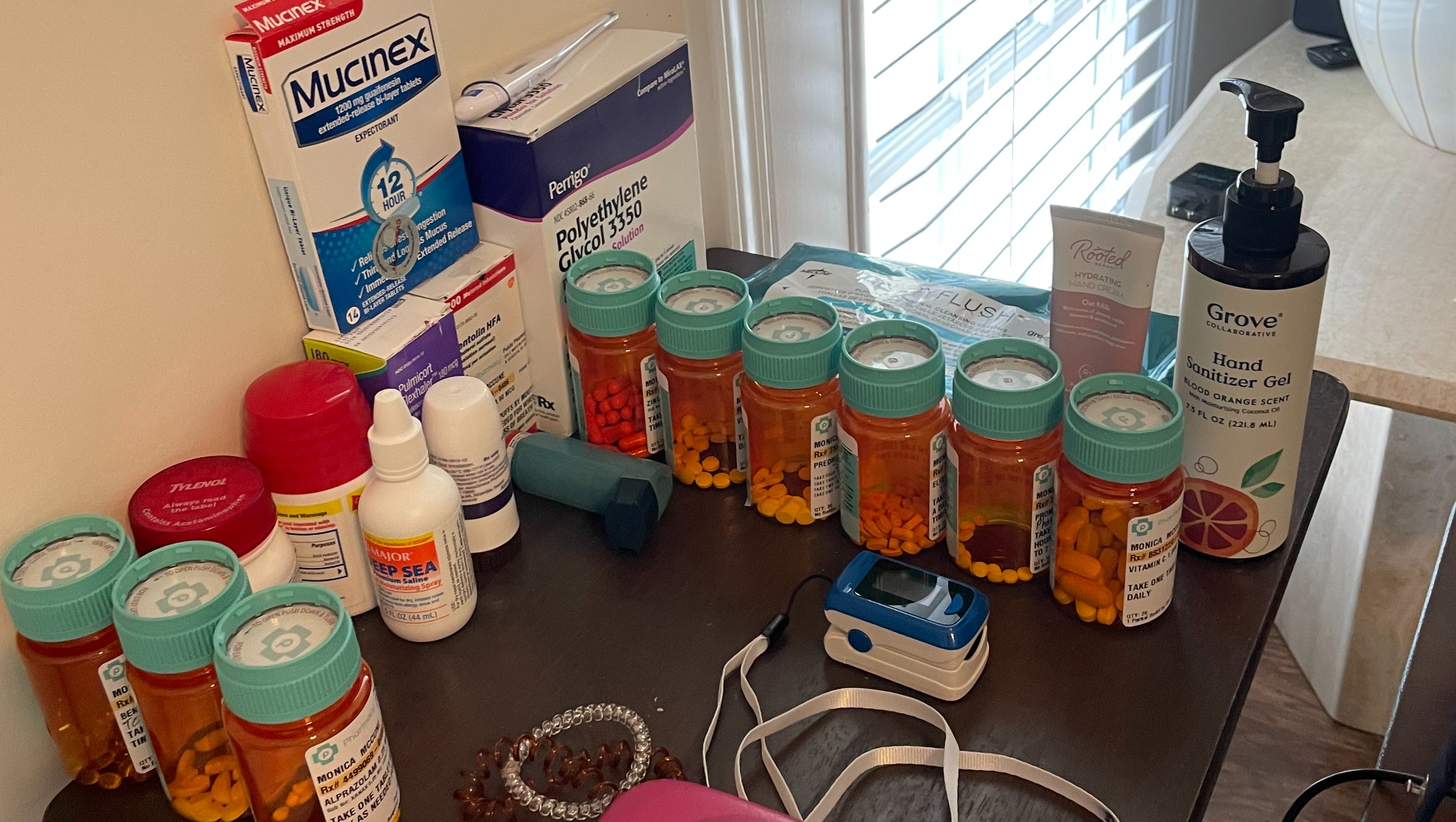
All my medications currently taking
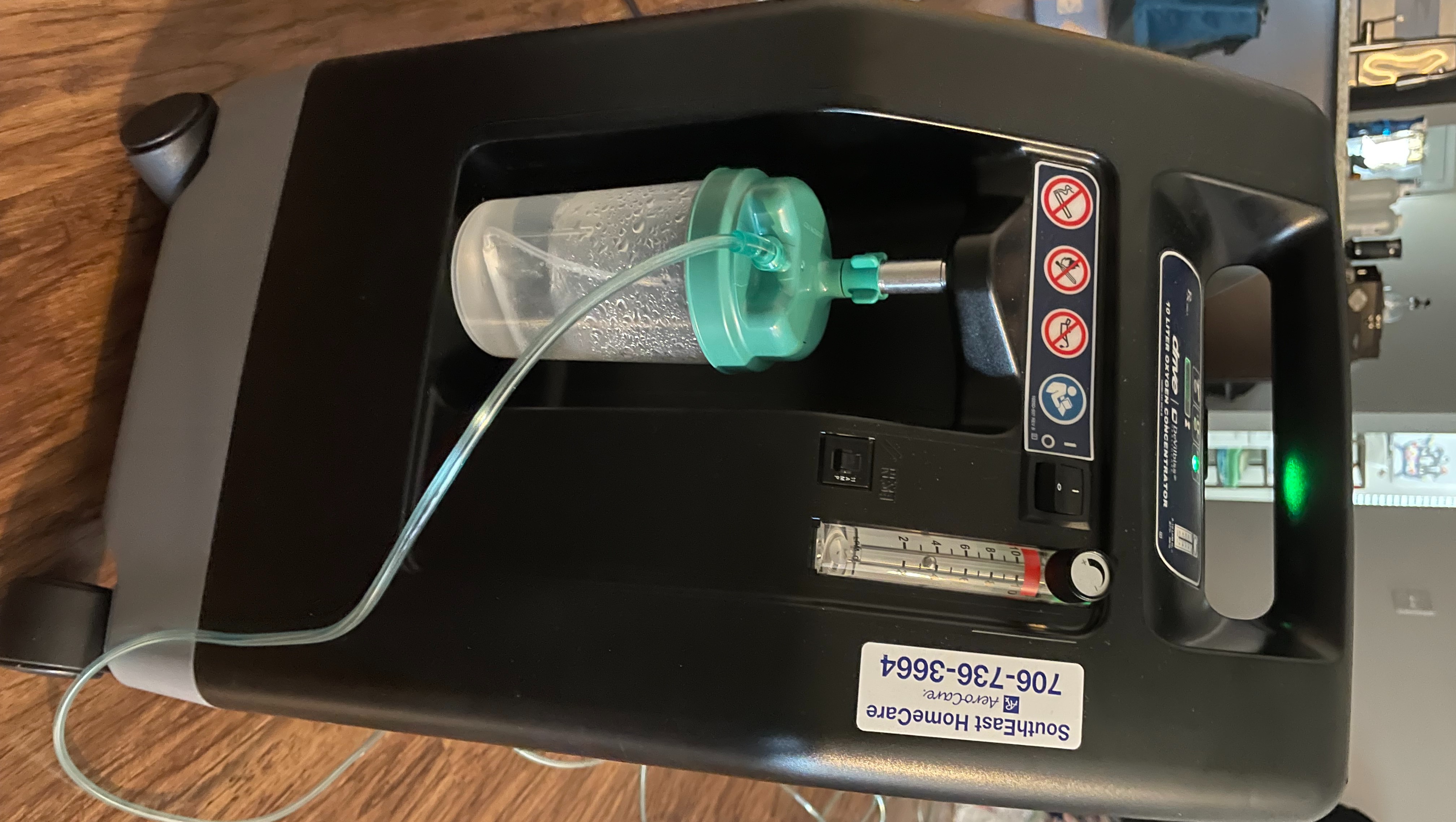
My best friend: oxygen concentrator I am tethered to 24/7 ( the bottle is what EMS gave me)

High flow oxygen and non-rebreather mask, the first few days of hospital when i was at my worst

Second day HOME SWEET HOME

Kiki, my little old lady who is spoiled and well taken care of!

Portable concentrator I'm working on getting as to not to have to travel with oxygen tanks when one tank only last an hour at my settings

Released from COVID isolation and moved to regular floor. The 10th floor view from my new room.

My snack I couldn't get enough of and one of the few things that tasted good once I gained my taste some
Organizer
Monica McCune
Organizer
North Augusta, SC