The Headstrong Project describes itself as a non-profit mental health organization that provides confidential PTSD treatment to veterans, service members and family (Headstrong, est. 2012).
PTSD affects many veterans, active-duty members, and their loved ones, whether or not they have experienced combat (Silvestrini & Chen, 2022). In their research, Silvestrini and Chen note, “Among the U.S. military veteran population, PTSD is one of the most prevalent mental disorders, with studies estimating PTSD rates ranging from approximately 8% to 22%” (2022). Despite these high percentages, plenty of veterans avoid treatment.
Focusing first on the experiences of men, it has been observed that “...male veterans may be reluctant to initiate PTSD care due to stigma, distrust of the military or mental health care, and a desire to avoid reliving their trauma” (Silvestrini and Chen, 2022).
Whereas it was found that women struggle with accessing VA care including everything from misunderstandings and lack of “women-specific health care” to outright discrimination and safety concerns (Evans et. al., 2019). Furthermore, “it is not uncommon for women veterans to use VA-provided health and social services as a ‘last resort’” (Evans et. al., 2024).
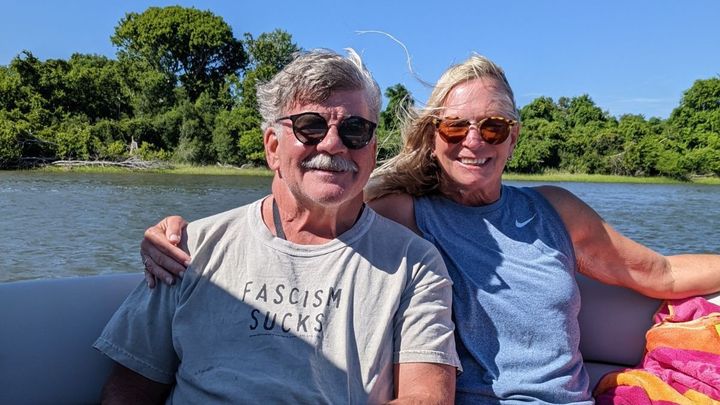
Left untreated, PTSD can lead to severe anxiety, depression, and suicide, which is why it’s important to have readily available and free resources for those in need. Mental health can be especially difficult for service members to tackle, when the only advice your training gives you is to ‘buck up’. We were lucky enough to work with someone who has a personal connection to these issues and who generously and bravely shared his experience. We include his story below.
One of our fundraising teammates has spoken with people who have used Headstrong’s services. Katie commented, “Typically, Headstrong reaches about 1,400 clients per month that are in need. Headstrong helps with anxiety, PTSD, depression, anger management, loss, and many other traumas. Clients that have been in the program have stated that Headstrong is a stigma and barrier free mental treatment facility for military, veterans, and their families” (2024).
We ask of you to please help us reach our goal of raising $500 to help support our troops and their loved ones regarding mental health services for PTSD! The money will go towards the Headstrong Project’s trauma treatments, providing assistance for clinical mental health services.
Our friend’s story:
After deploying in 2015, I returned home to the country that I fought very hard to defend. A loving wife and my 2-year-old daughter welcomed me home with open arms and lots of love. The first couple of months back on US soil was just like anybody else's; two weeks of leave, medical checks and slowly getting back to work. About three months after returning home, I slowly began to realize that something seemed out of sorts with myself but much like any good soldier, I took a knee, drank water, and drove on, just as we are instructed to do. It first began with waking up in the middle of the night, after a sudden noise. I would be startled awake, heart racing, palms sweating, with intrusive thoughts and uncontrollable shaking.
I fought it off and continued on, thinking it was a one-time thing. As time passed, all of the feelings and thoughts began to invade in my head on a much more regular basis. I kept experiencing nightmares that would shake me to my core, inevitably causing me to lose many hours of sleep per night. I would walk around the house, terrified to go back to sleep because I did not want to have them again. For months, I told my wife and my unit that everything was fine, that I was not struggling. This was my mindset because since I first joined the Army, I was always taught that good soldiers should always push forward and continue fighting. Although this was a battle I had never experienced before, I was willing to fight it and deal with it on my own. Unlike many other battles I have fought, I was very close to losing my battle with PTSD (Post-Traumatic Stress Disorder) and it almost cost me my life.
Just like any other night, we first put my daughter to bed and then my wife and I were getting ready ourselves. My wife knew something was off, so she asked me, “Are you okay?” I responded like I normally did, knowing what I was planning to do after she fell asleep. Over the next hour, she kept on me until I finally broke down and told her that I was going to take my life by taking enough medications (that were prescribed to me), hoping that I would not wake up. She immediately called a fellow NCO to come to my house and help me because she did not know how to exactly help me. At 2300 that night, he showed up, loaded me in his truck, and we went to the Emergency Room. I do not remember much from that night, although I vividly remember being sent to the in-patient wing of the hospital where they kept me for 3 days. Immediately following that, I was put into an Intensive Out-Patient program that specifically handled PTSD. I did that for several weeks and continued treatment with the Mental Health Clinic on post. After about 7 months, they recommended me for a Med-Board, I began the process and was medically retired from the military.
My family and I moved to Colorado where I started “treatment” with the VA and did many forms of therapy to try to help me fight against PTSD, but to no avail. I went into a zombie-like trance where I was depressed, scared to leave my house, and anxious about doing anything outside my normal routine. This continued and once again, I said I was fine, that everything was okay. Although the suicidal ideations were still very real to me, I felt that I had to put on a brave face for everyone around me and continue being the strong soldier I was made to be.
I was having a lot of difficulty internally at the workplace, my household, adjusting to civilian life, and trying to feel like a human being. This did reprehensible damage to my wife’s and I relationship and over time. I think we both realized that she had so much resentment built up towards me for putting her through that it could not recover.
Although I did not ask to get PTSD, she also did not ask to be on the other side of being with someone that has it. The mental and physical exhaustion that my wife went through to ensure my safety should not be expected from anyone, but she did it as bravely as she could. The countless nights she would wake up to check if I was still breathing took its toll over time and I will always feel a level of guilt over putting her through that during that time of my life.
Over time, my PTSD did not get any “better”, I just learned how to deal with it. It took many years to get where I am today all while still struggling with PTSD daily. I still can not go to busy places. When I go out, I always have my back in a corner at restaurants so I can see the whole restaurant and even go to measures such as taking different roads to and from work.
I learned over time that even though I struggle with this mental health condition, there are ways to mitigate its effects by putting safety measures in place so I can still attempt to enjoy life. A part of me wonders if I would have said anything earlier, would I still be on active duty? Would I still be able to teach and train our future generations of soldiers? Would I still be able to go play in the sandbox? Would I still be a part of America's greatest traditions?
I loved being a soldier more than anything and to this day, I wish I could have stayed in and progressed my career, shaping young soldiers’ lives for the better. Unfortunately, I was part of the stigma and did not say anything. Speaking out was a sign of weakness and I did not want to appear weak to anyone. So, again, I did what I always have, and I took a knee, drank water, and drove on. That is until I couldn’t anymore. I was fighting a losing fight by myself along with my pride and selfishness to be the best and it played an instrumental part in me almost taking my own life. I could not deal with the invisible pain I was fighting against and taking my own life seemed worth it at the time. I almost became another soldier losing his own life to PTSD because of my pride.
So, I say to whoever reads this, you are not alone, do not become a statistic, do not let pride tear you down, do not be afraid to speak up because like mine, your life may depend on it! Always remember that when fighting an invisible fight, it may be in your head, but you indeed are not alone. There are many of us out there that would move mountains to ensure fellow soldiers’ health and safety. Active, Retired, Discharged or Reserve, it doesn’t matter. We are brothers and sisters in arms until we take our last breath on this earth, and we always have each other’s 6. HOOAH!!!
If you would like to learn more about the Headstrong Project and its reach please visit Our Reach - The Headstrong Project where it shows yearly data concerning client growth, session growth and number of clinicians as well as their clinical network locations. For more general information and other ways to help, please visit The Headstrong Project or contact [email redacted].
Reference List
Anonymous Friend. (2024).
Evans, E. A., Tennenbaum, D. L., Washington, D. L., & Hamilton, A. B. (2019). Why Women Veterans Do Not Use VA-Provided Health and Social Services: Implications for Health Care Design and Delivery. Journal of Humanistic Psychology, 64(2), 002216781984732. https://doi.org/10.1177/0022167819847328
Headstrong. (est. 2012). About Headstrong. The Headstrong Project. Retrieved April 19, 2024, from https://theheadstrongproject.org/about/
Hinton, M., Metcalf, O., Varker, T., Roebuck, G., McGaw, V., Watson, L., Fredrickson, J., Johnson, L., Forbes, D., Phelps, A., Dzenana Kartal, Dell, L., Bryant, R., McFarlane, A. C., Hopwood, M., & O’Donnell, M. (2022). A Qualitative Study of the Expectations, Experiences, and Perceptions That Underpin Decisions Regarding PTSD Treatment in Help-seeking Veterans. Military Medicine, 188(7-8), e2234–e2241. https://doi.org/10.1093/milmed/usac374
Silvestrini, M., & Chen, J. A. (2022). “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care.. Psychological Trauma: Theory, Research, Practice, and Policy, 15(4), 665–671. https://doi.org/10.1037/tra0001382